Translate this page into:
Epithelial hyperplasia: A clinical mirage of a histopathological entity

*Corresponding author Dr. Saramma Mathew Fenn, MDS, PhD, Associate Professor, Department of Oral Medicine and Radiology, Vinayaka Mission’s Sankarachariyar Dental College, Vinayaka Mission’s Research Foundation (Deemed to be University), Salem, Tamil Nadu, India. drsarammamathewfenn@vmsdc.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Sruti S, Fenn SM, Jacob M, Priya S, Viggness A, Subramanian M. Epithelial hyperplasia: A clinical mirage of a histopathological entity. J Academy Dent Educ. 2023;9:94-6. doi: 10.25259/JADE_2_2023
Abstract
Epithelial lesions that mimic infectious disease, a reactive lesion, or a neoplastic entity are frequently encountered by dentists, especially specialists in Oral Medicine and Radiology. Improper or incomplete history can complicate clinical differentials even further, leading dentists to prescribe medications that are frequently unnecessary. The histological diagnosis obtained after a biopsy is usually conclusive when representative tissue is incised and sent for diagnosis. This case report presents an intriguing case of a patient with papillary growth along the midline of the palate that was histologically diagnosed as epithelial hyperplasia, which describes the nature of the lesion but masks the clinical symptoms of the underlying inflammatory papillary hyperplasia.
Keywords
Epithelial lesions
Inflammatory papillary hyperplasia
Nodular candidiasis
INTRODUCTION
Epithelial lesions, commonly encountered by dentists, can present clinically in a myriad of clinical forms due to their inherent ability to adapt and multiply in response to any external agent, whether a microorganism, chemical exposure, or physical agent. This adaptation causes basal cells to proliferate, increasing the number of layers and the thickness of the overlying keratotic layer in an attempt to protect the underlying connective tissue from such agents. Such adaptations, however, are triggered by nuclear and cytoplasmic interactions and can manifest clinically and histologically as epithelial hyperplasia.
This article presents an intriguing case of a patient with inflammatory papillary hyperplasia (IPH) presenting as a papillary growth, necessitating the need to rule out a number of possible differential diagnoses that, if not biopsied, would be misdiagnosed and treated incorrectly.
CASE REPORT
A 78-year-old male presented to the Department of Oral Medicine and Radiology complaining of pain in the left back tooth region. The patient makes no mention of a burning sensation or a dental history of wearing a prosthesis. History also revealed the habit of beedi smoking of around with 5–6 beedis/day for the past 10 years. During the extraoral examination, no lymph nodes were palpable. Intraoral examination revealed 3 × 5 cm erythematous papillary growth along the central region of the hard palate in the mid-palatal raphae behind the premaxilla. As shown in Figure 1a, the lesion extends 2 mm away from the rugae of the anterior part of the hard palate, 8 mm away from the uvula, and 4 mm away from the posterior alveolar ridge region. On palpation, the papillary growth was firm, immobile, and fixed to the underlying structures, with a sessile base and no tenderness.
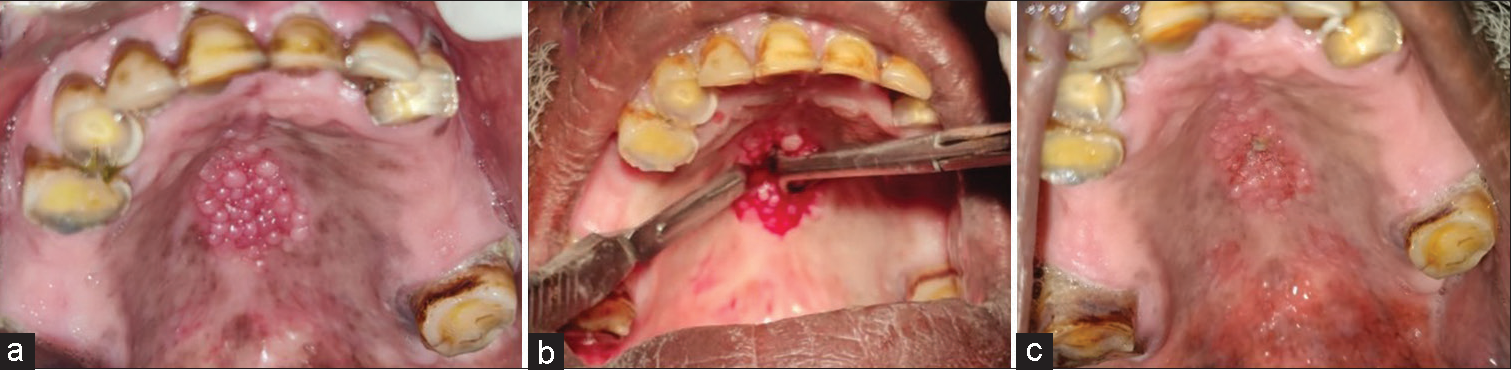
- (a) Papillary growth along the mid-palatal raphe, (b) incisional biopsy, (c) and postoperative photograph after 1 week.
A provisional diagnosis of nodular candidiasis was made based on the clinical appearance. Due to the varied clinical appearance, site and history of tobacco use, nicotine stomatitis, denture stomatitis type III, and Heck’s disease were considered as differential diagnoses. Figure 1b show an incisional biopsy performed under local anesthesia and sent for histopathological examination. Figure 1c shows the post-biopsy wound after 1 week. The papillary pattern of growth seen clinically can be appreciated in the specimen and low power view of the histological section, as shown in Figure 2a-c. The specimen showed a proliferating parakeratinized stratified squamous epithelium and cellular connective tissue. The epithelium is characterized by pseudoepitheliomatous hyperplasia and the connective tissue beneath is loose and fibrillar, revealing blood vessels and inflammatory cells [Figure 2d]. The final diagnosis was inflammatory epithelial hyperplasia based on the histological findings.
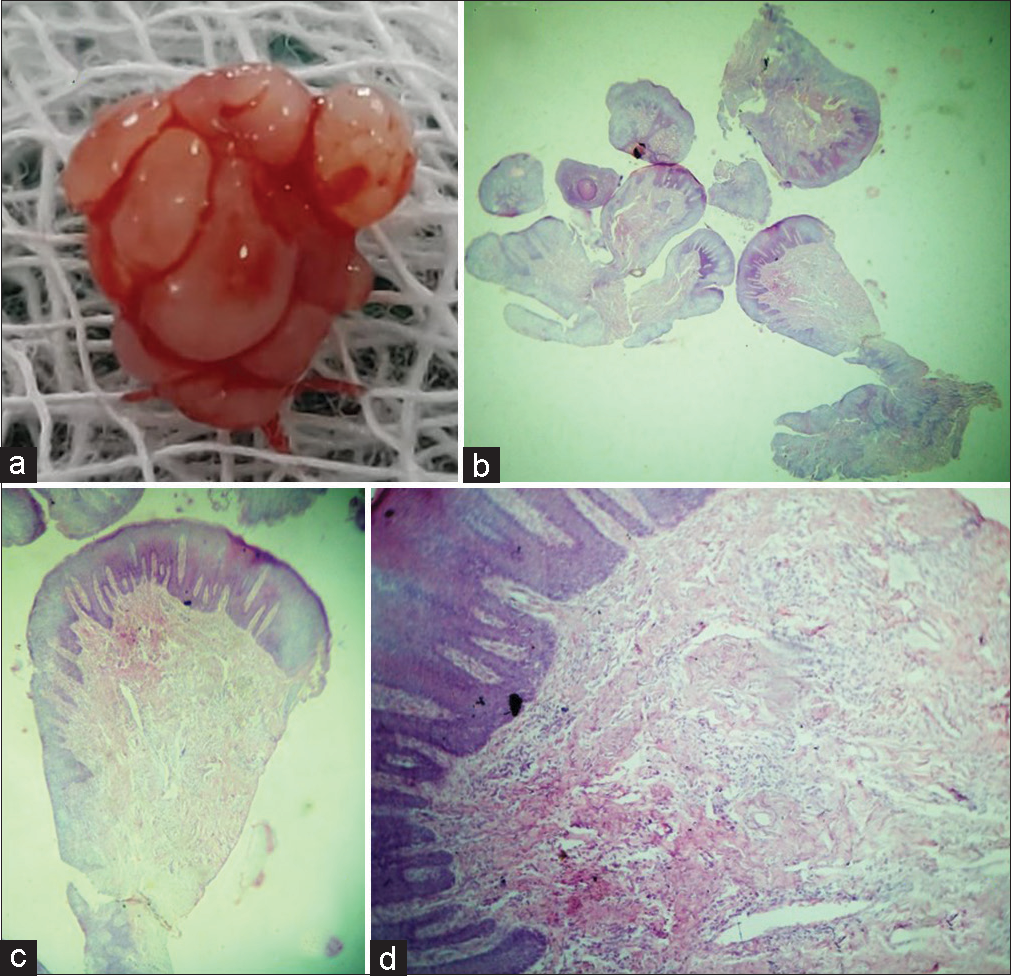
- (a) Biopsy specimen showing the papillary pattern of growth appreciated clinically, (b and c) photomicrograph of papillary growth, H and E, ×0.7, ×1, and (d) photomicrograph showing parakeratinized stratified squamous surface epithelium and underlying highly cellular stroma with chronic inflammatory cells. H and E, ×20.
DISCUSSION
The oral mucosa is continually exposed to external and internal stimuli, resulting in a variety of disease conditions ranging from inflammatory reaction, developmental, and neoplastic. Inflammatory hyperplasia, also known as papillary hyperplasia of the palate; palatine papillomatosis that occurs exclusively on the central palate, is one such reactive lesion. These are responses of benign soft tissues to a local irritant that are commonly associated with denture wear, soft and hard tissue deposits such as calculus, sharp cusps of a tooth, a fractured filling, and other aggravating factors.[1] The earlier stage of the lesion appears erythematous, soft and bleeds easily. When it becomes fibrosed, it takes on a firm, pink appearance, similar to the present case.[2] Because clinically, oral mucosal lesions resemble other epithelial hyperplasias, like IPH must be recognized.
IPH of the palate in non-denture wearers is uncommon, and one such occurrence was observed in our case. The lesion was asymptomatic, and the color of the mucosa ranged from pink to red and papillary in appearance. The patient had no history of wearing a dental prosthesis. We found only two cases of IPH in non-denture-wearing patients in the literature, which were attributed to poor oral hygiene, smokers, and/or mouth breathers. Consideration of maxillary denture may not be the singular cause of the appearance of such a lesion.[3,4]
Chronic trauma can induce an inflammatory reaction, which most often results in granulation tissue with accompanying endothelial cells, chronic inflammatory cells, and later fibroblasts proliferating and manifesting as reactive hyperplasia or focal reactive overgrowths. Although these lesions have no malignant potential, they represent a chronic process in which an exaggerated reparative mechanism or the adaptive response of oral tissue to low-grade chronic irritation occurs. Early detection and removal of these lesions, as well as the removal of the irritant, can greatly reduce the risk of dentoalveolar complications.[5,6]
Considering the patient had the habit of smoking, the possibility of nicotine stomatitis could be considered due to the heat generated from the habit of using the tobacco product, there would be an inflammatory reaction of the minor salivary glands in the palate which will give rise to papillary appearance as seen in this case. However, such a papular appearance will elicit reddish dots in the center, which can be distinguished from papillary hyperplasia. Furthermore, on cessation of the habit, the lesion is completely reversible and would resolve within a period of a few weeks.[7]
Another inflammatory lesion to be considered in the differential diagnosis based on the location is denture stomatitis type III which can be ruled out with dental history. The possible etiology of ill-fitting is seen with a clinical appearance of multiple smooth granular appearances on the alveolar ridge and pre-maxilla region, which can be distinguished with the dental history seen in this case, where the patient gave a negative dental history of wearing a denture.
Focal epithelial hyperplasia or Heck’s disease is a viral-induced epithelial proliferation that manifests as multiple rounded papules similar to the present case but is frequently distinguished by the appearance of papules coalescing to form a cobblestone appearance.[8,9] Although a papillary lesion had been identified in this case, it did not exhibit the usual characteristic of multiple clusters of lesions that did not merge despite being present for a period of time.[10] Furthermore, in the histological features of elongated rete, ridges with mitosoid bodies were not observed in the present case.
Candidiasis nodularis (classification proposed by Samaranayake) manifests as erythematous nodules with an overlying whitish plaque that can be rubbed off.[11,12] In this case, the patient was asymptomatic and was unaware of such changes in the mucosa and the features did not correlate with histological findings.[13] The patient was advised to stop smoking and was watched for regression in the size of the lesion.
CONCLUSION
The clinical appearance of lesions in the oral cavity frequently masquerades the histological features of a lesion. As a result, earlier and more accurate diagnosis improves the quality of life and patient care. To avoid misdiagnosis and incorrect treatment, the dentist must be aware of all such types of lesions that have no malignant transformation potential.
Ethical approval
The research/study complied with the Helsinki Declaration of 1964.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Inflammatory hyperplasia: From diagnosis to treatment. J Indian Soc Periodontol. 2014;18:92-4.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory fibro-epithelial hyperplasia related to a fixed implant-supported prosthesis: A case report. J Clin Exp Dent. 2018;10:e945-8.
- [CrossRef] [PubMed] [Google Scholar]
- Focal fibrous hyperplasia: A review of 193 cases. J Oral Maxillofac Pathol. 2014;18:S86-9.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory papillary hyperplasia: A systematic review. Med Oral Patol Oral Cir Bucal. 2017;22:36-42.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory papillary hyperplasia of the oral mucosa: Report of 341 cases. J Am Dent Assoc. 1970;81:949-52.
- [CrossRef] [PubMed] [Google Scholar]
- Reactive hyperplastic lesions of the oral cavity: A ten year observational study on North Indian Population. J Clin Exp Dent. 2012;4:e136-40.
- [CrossRef] [PubMed] [Google Scholar]
- Constellation of oral inflammatory hyperplastic lesions: Case series with review of literature. Int J Med Res Health Sci. 2019;8:101-6.
- [Google Scholar]
- Oral multifocal epithelial hyperplasia: An unusual entity. Int J Appl Basic Med Res. 2019;9:253-5.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology and management of inflammatory papillary hyperplasia in completely edentulous patients-a review. J Curr Med Res Opin. 2020;3:614-8.
- [CrossRef] [Google Scholar]
- Candidiasis-oral manifestations: A literature review. Int J Sci Res. 2021;10:568-71.
- [Google Scholar]
- Isolation and identification of Candida from the oral cavity. ISRN Dent. 2011;2011:487921.
- [CrossRef] [PubMed] [Google Scholar]
- Oral erythematous candidiasis: A case report. Int J Med Dent Case Rep. 2020;7:1-4.
- [CrossRef] [Google Scholar]







