Translate this page into:
Periodontal application of ozone therapy

*Corresponding author: Arushi Tyagi, Intern, Subharti Dental College, Merrut, Uttar Pradesh India. arushityagi109@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tyagi A, Khattri S. Periodontal application of ozone therapy. J Academy Dent Educ. 2023;9:80-5. doi: 10.25259/ JADE_63_2022
Abstract
The prevalence of periodontium-related problems has been rising globally, impacting individuals across various age groups. Hence, it is crucial for the medical fraternity to address the treatment and subsequently prioritize prevention of the same. Periodontal infections involve the invasion by various bacterial inhabitants deep within the healthy pockets, leading to progressive recession with bone loss and tooth mobility, resulting in periodontitis. Therefore, effective decontamination of periodontal pockets is of paramount importance. Ozone, a natural constituent of the earth’s atmosphere, has now revolutionized the field of medicine since its introduction. Due to its highly unstable and oxidizing form, its procurement and implementation of ozone were challenging initially. The recent advancement in technologies has made it possible to stabilize ozone, enabling comprehensive approaches to major ailments. This literature review intends to illustrate ozone therapy and its diversified application as an adjunct in surgical and nonsurgical periodontal therapies. Ozone therapy has proven its potentiality by promising faster tissue regeneration, aiding in wound healing to effectively decontaminate the pocket depths, resulting in a successful prognosis. The review explores diverse systems and products used for ozone generation across different modalities, with limitations of the same. Evidence provided in the literature will contribute to a better understanding of ozone therapy’s role in improving periodontal health and guide future research in this field.
Keywords
Ozone therapy
Non-invasive
Tissue regeneration
Periodontal diseases
INTRODUCTION
Periodontal disease is a chronic inflammatory response of the periodontium surrounding teeth, leading to irreversible damage to the periodontal ligament with progressive destruction of alveolar bone in advanced stages. Periodontal-related diseases are the most common oral condition in the human population. The prevalence of periodontal diseases affects about 20–50% of the population globally.[1] This condition is considered one of the two core threats to the oral cavity, leading to tooth loss.[2] The percentage of affected adolescents in developing countries ranges from 35% to 70%, whereas in developed nations the affected ranges from 4% to 34%. The percentage of the affected adult population in developing countries ranges from 36 to 63%, with 14–47% of the affected adult population in developed countries. These diseases have shown an increased predilection for geriatric patients, with periodontal pockets of 6 mm or above in both developed and developing countries.[3] Due to the chronic nature of the disease, it becomes imperative to restrict its severity and prevalence through a comprehensive treatment planning and an effective prophylactic approach of the same. One such recent discovery involves, ozone therapy administered in either aqueous or gaseous form. Being a potent oxidizing agent with high biocompatibility, this non-invasive treatment modality is been widely used in various fields of interest, including medicine, dentistry, and veterinary medicine.[4] The studies discussed below in this literature review will focus on the biological efficiency of ozone with inferences from various studies confirming the same, particularly in surgical and non-surgical procedures concerning the field of periodontology when used as a supplement.
HISTORY
The word “OZONE” took its origin from the Greek word ozein meaning “to smell.” Ozone was originally discovered by a Dutch chemist, Martinus van Marum, in 1785 while conducting electric sparking over water, when he noted a distinct smell, only to acknowledge later the smell being of ozone. A half-century later, it was Christian Friedrich Schobein, who theorized the presence of ozone.[5]
Ozone was first implicated in the medicinal field by Landler in 1870. However, it was in 1936 that it was taken under serious consideration by a Swiss dentist, Dr. E. A. Fisher,[6] where it was studied in the form of ozonated water and put into use during his daily practice. It was when one of his patients, Dr. E. Payr was getting treated for a gangrenous pulpite that and developed a great sense of interest in the local action of ozone during his treatment of the disease and later extended its application.
In 1957, Joachim Hänsler and Hans Wolff, German physicists, developed the first ozone generator for medical usage, which now continues to be a basis for modern medical-grade ozone generators.[7]
BIOLOGICAL ACTION UNDERTAKEN BY THE OZONE ADMINISTRATION
This non-invasive treatment modality is now used as an adjunctive or preventive treatment, resulting in successful prognoses in the field of medicine, which is now gaining popularity. Ozone therapy is well known for its antibacterial activity along with its anti-hypoxic effect and has proven its efficacy in immune stimulatory activity as well. The following are the biological actions undertaken by the ozone administration:
Antimicrobial action
Ozone is proven to be highly effective in the destruction of microorganisms such as bacteria, viruses, and fungi. The ozone directly acts on the cell membranes in these cases. In bacteria, it acts directly on the cytoplasmic membrane by ozonolysis of the dual bond duality with the ability to modify the intercellular contents through oxidation of the proteins in various organelles within the bacteria. This act is non-specific and selective in nature, where Gram-positive shows more sensitivity to ozone than Gram-negative. The potency of action increases in the presence of a liquid medium with an acidic pH. This action is selective to microbial cells but does not damage the body cells because of their major anti-oxidative ability.[8] Ozone has shown to be competent toward the viral sheaths, where it acts on the multi-unsaturated fatty acids chains of the lipid sheath and disintegrates the viral sheath.[9]
Immune stimulating action
Various studies concluded the immune stimulating effect influences both the humoral and the cell-mediated immune systems.[8] The ozone functions by activating the macrophages, stimulating the release of certain chemical mediators such as cytokine, setting in action a cascade of biochemical reactions, and resulting in the production of various anti-inflammatory mediators such as leukotrienes, interleukins, and prostaglandins. Thus decreasing the inflammation and aiding in effective wound healing.[8] In high concentrations, ozone acts by depressing immune activity, whereas in cases of low concentration, it increases immune activity.[9]
Anti-hypoxic action
Ozone has been shown to elevate the pO2 levels in tissues and improve oxygen transportation throughout. In repetitive low doses, it protects the calls against oxygen free radicals by activating various enzymes such as superoxide dismutases, catalases, dehydrogenases, and glutathione. It also prevents the aggravation of erythrocytes and increases the contact surface area for the attachment of oxygen, for better transportation.[8] Ozone also improves the metabolism of inflamed tissues by reducing local inflammation and potentiating the oxidation process.
Biosynthetic action
By influencing the biochemical processes within the cells, it stimulates protein synthesis and thus increases the amount of ribosomes and mitochondria within. At the cellular level, this explains the regenerative potentiality of the tissues and organs post-ozone therapy.[8] It also aids in the activation of angiogenesis.[9]
GENERATION OF OZONE
Medical grade ozone is used in the ratio of 0.05–5% of O3 and 95–99.95% of O2. Due to the unstable nature of ozone, it is to be manufactured freshly before the treatment. The three systems used for the generation are as follows: [10]
Ultraviolet system
Ozone is created by the photolysis of the O2 molecule by ultraviolet light in the range of 160–240 nm, producing a low concentration of ozone, commonly implicated in air purification or esthetic treatment modalities.
Corona discharge system
The system results in the cleavage of the oxygen molecule as two oxygen radicals, thus producing a high concentration of ozone. This is the most common form of ozone generator. Used in the medical/dental field.
Cold plasma system
This utilizes oxygen as the input source and is used to produce ozone in the concentration of 5–7%. Used in air and water purification systems widely.
MANUFACTURE OF OZONE IN DENTISTRY
The table 1 mentioned below has stated the various manufacturing industries responsible for medical grade ozone producing devices, with a holistic overview of the same.
| Product | System used | Form | Advantages | Disadvantages |
|---|---|---|---|---|
| Ozonette DENT (Sold by Sedecal)[11] |
Corona discharge system | Gaseous form |
|
|
| Ozonytron-XPO (MIO Int. OZONYTRON GmbH)[12] |
Cold plasma system | Gaseous form |
|
|
| Ozonsan cytozon (Hansler Medical)[13] | Normobaric infusion therapy (ozonized water) | Aqueous form |
|
|
| OxActiv (ozonated olive oil gel)[14] |
Infused ozone in gel based product | Aqueous gel |
|
|
AOD: Automatic overpressure detection. Manufacture of ozone in dentistry
SAFETY PRECAUTIONS AND GUIDELINES FOR HANDLING
Ozone, when administered in its gaseous form, without any proper administration specification, can source ozone toxicity via inhalation. Has been known to show the following side effects mentioned below:[10]
Epiphora
Upper respiratory tract irritation
Rhinitis
Cough
Headache
Occasional nausea.
Adversities caused either by leakage or unmoderated gaseous doses can potentially result in ozone intoxication. The following must be performed, immediately:[10]
The patient must be placed in a supine position
Inhalation of humid oxygen
Administration of ascorbic acid, Vitamin E, and N-acetylcysteine [Figure 1].
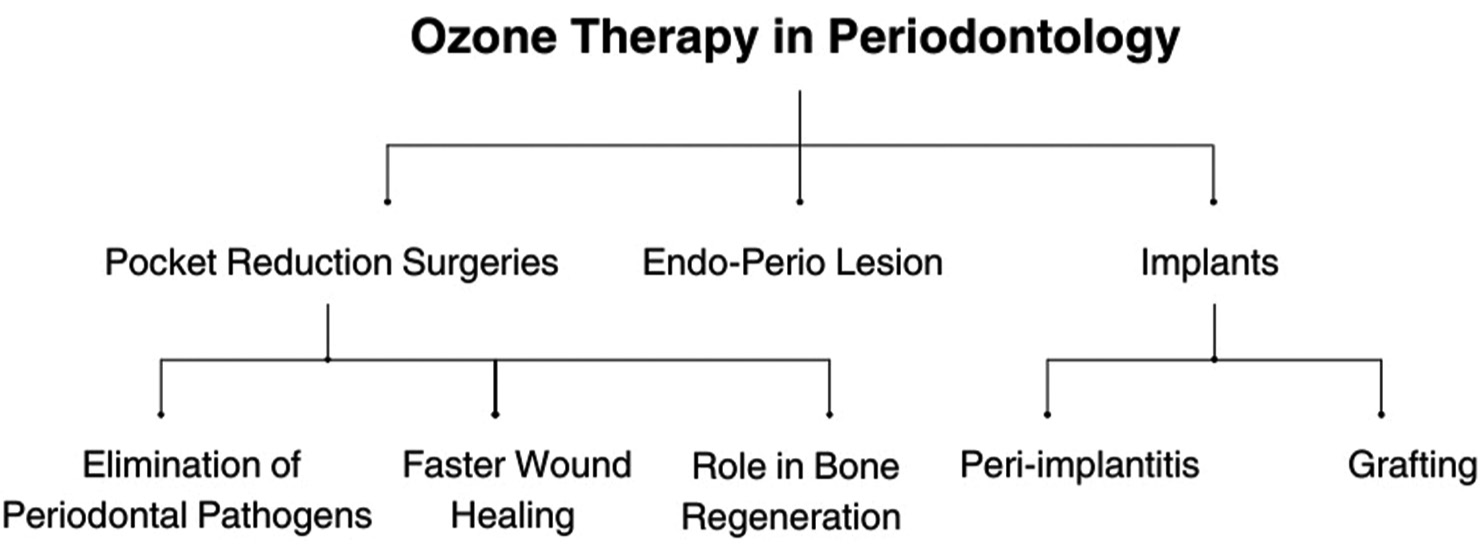
- Ozone therapy in periodontology.
EVIDENCE OF OZONE APPLICATION IN PERIODONTOLOGY
The table 2 mentioned below is an assemblage of various studies conducted regarding the application of ozone therapy and its results in applied periodontolgy with Inferences of the same.
| Author and year of publication | Use of ozone | Inference of the study conducted |
|---|---|---|
| Huth et al. 2007[15] | As an antiseptic agent. As a pre-surgical mouth rinse. |
The study confirmed the aqueous form of ozone as a potential antiseptic agent with low cytotoxicity for oral application. |
| Filippi[16] | As an irrigant post-surgical procedures for swift healing of the wound. | The study concluded an accelerated wound healing in the oral mucosa within the first 48 h with ozone water. |
| Nagayoshi et al. 2004[17] | As an irrigant peri dental procedure. As a mouth rinse |
The study concluded the bactericidal effect of ozonated water over oral biofilm with a predilection for Gram-negative bacteria in vitro. |
| Hems et al. 2005[18] | As an irrigating agent. | Tested the efficacy of aqueous and gaseous forms of ozone against Enterococcus faecalisin biofilm. |
| Kshitish and Laxman 2010[19] | As an irrigating agent, to reduce pocket depth. As mouth rinse. |
The study interpreted a higher percentage in reduction of plaque index, gingival index, and bleeding index with the use of ozonated water in comparison with CHX, with percentile reduction in aggregatibacter actinomycetemcomitans (Aa) in patients of chronic generalized periodontitis. |
| Ramzy et al. 2005[20] | As an irrigant during the treatment of aggressive periodontitis | The study conducted in patients suffering from aggressive periodontitis was irrigated once weekly with 150 mL of ozonated water, concluding a significant reduction of bacterial count in periodontal pockets. |
| Hauser–Gerspach et al. 2012[21] | As a sterilizing agent prior to implant placement in the oral cavity, reducing chances of peri-implantitis. | The study concluded the antimicrobial efficacy of gaseous ozone against bacteria adherent over titanium and zirconia dental implants, without affecting the adhesion and proliferation of the osteoblastic cells. |
| Ebensberger et al. 2002[22] | As a cleaning agent and for root surface decontamination for an avulsed tooth reimplantation. | The study concluded the 2-min irrigation with isotonic ozonated water decontaminated the root surface with on deteriorating effect over the periodontal cells viable over the root surface, along with mechanical cleaning. |
Evidence of ozone application in periodontology
CONTRAINDICATIONS OF OZONE THERAPY IN PERIODONTOLOGY
The following mentioned below are some of the contraindications, during the administration of ozone therapy:[10]
Pregnancy, particularly the early phase, excludes any mutagenic risk, although it is unlikely[23]
Glucose-6-phosphate-dehydrogenase deficiency (G-6-PD) (favism): The enzyme G-6-PD is crucial for eliminating equivalents able to abolish excessive oxidation and intensive hemolysis. Deficiency of the same, results in hemolytic disease known as favism. On exposure to ozone, it is associated with the precipitation of acute hemolysis in such cases[24]
Hyperthyroidism: The sensitivity of the lung to damage due to ozone therapy may be highly dependent on an individual’s thyroid hormone status. The chances of aggravation of the lung toxicity in patients with a hyperthyroid state are more likely[25]
Severe anemia
Severe myasthenia gravis
Active hemorrhage
Acute alcohol intoxication
Recent myocardial infarction.
CONCLUSION
Ozone has wide application in both medical and dental fields due to its various benefactors aiding in faster healing processes and disinfection has proven to be an efficient adjunct to conventional surgical procedures. Due to its simplicity of usage, it has no side effects and has been shown to have good tolerance among patients and economic efficiency thus becoming a popular modality. In periodontology, this modality is used effectively in the treatment of peri-implantitis, disinfection of periodontal pockets, regeneration of bone, and speeding the process of wound healing post surgeries.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- European workshop in periodontal health and cardiovascular disease-scientific evidence on the association between periodontal and cardiovascular diseases: A review of the literature. Eur Heart J Suppl. 2010;12(Suppl B):B3-12.
- [CrossRef] [Google Scholar]
- Periodontitis in systemic rheumatic diseases. Nat Rev Rheumatol. 2009;5:218-24.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of periodontal disease, its association with systemic diseases and prevention. Int J Health Sci. 2017;11:72.
- [Google Scholar]
- Ozone In: Wikipedia. The Free Encyclopedia. 2023. Available from: https://en.wikipedia.org/w/index.php?title=Ozone&oldid=1163068546 [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Apparatus for production and use of ozone in therapeutics Filed April 5, 1934 Patented Sept.15, 1936, Serial No. 119,214. Available from: https://patents.google.com/patent/US2054367A/en [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Applications of ozone therapy in dentistry. J Oral Res Rev. 2016;8:86-91.
- [CrossRef] [Google Scholar]
- Ozone and its usage in general medicine and dentistry. A review article. Prague Med Rep. 2008;109:5-13.
- [Google Scholar]
- Practical use of ozone in dentistry-comments. Ann Univ Mariae Curie Sklodowska Lubin Polonia. 2008;63:28.
- [CrossRef] [Google Scholar]
- Ozone therapy in medicine and dentistry. J Contemp Dent Pract. 2008;9:75-84.
- [CrossRef] [PubMed] [Google Scholar]
- Ozonette dental system - medical ozone research institute. Medical Ozone Research Institute. Available from: https://medicalozoneresearchinstitute.org/ozonette-dental-system [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Plasma therapy and ozone therapy - differences and effects. Available from: https://www.ozonytron.com/en/plasma-therapy/plasma-and-ozone [Last accessed on 2023 Jul 03]
- [Google Scholar]
- Ozone water in dentistry. Available from: https://hoffmann-dental.com/wp-content/uploads/2020/05/Ozone_EN_small.pdf [Last accessed on 2023 Jul 03]
- [Google Scholar]
- The effects of subgingival application of ozonated olive oil gel in patient with localized aggressive periodontitis. A clinical and bacteriological study. Tanta Dent J. 2014;11:63-73.
- [CrossRef] [Google Scholar]
- Effect of aqueous ozone on the NF-κB system. J Dent Res. 2007;86:451-6.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of ozonised water on the epithelial wound healing process in the oral cavity In: Clinic of oral surgery, radiology and oral medicine. Switzerland: University of Basel; 2001. Available from: https://www.oxyplus.net [Last accessed on 2022 Oct 14]
- [Google Scholar]
- Efficacy of ozone on survival and permeability of oral microorganisms. Oral Microbiol Immunol. 2004;19:240-6.
- [CrossRef] [PubMed] [Google Scholar]
- An in vitro evaluation of the ability of ozone to kill a strain of Enterococcus faecalis. Int Endod J. 2005;38:22-9.
- [CrossRef] [PubMed] [Google Scholar]
- The use of ozonated water and 0.2% chlorhexidine in the treatment of periodontitis patients: A clinical and microbiologic study. Indian J Dent Res. 2010;21:341-8.
- [CrossRef] [PubMed] [Google Scholar]
- Management of aggressive periodontitis using ozonized water. Egypt Med JNRC. 2005;6:229-45.
- [Google Scholar]
- Influence of gaseous ozone in peri-implantitis: Bactericidal efficacy and cellular response. An in vitro study using titanium and zirconia. Clin Oral Investig. 2012;16:1049-59.
- [CrossRef] [PubMed] [Google Scholar]
- PCNA-expression of cementoblasts and fibroblasts on the root surface after extraoral rinsing for decontamination. Dent Traumatol. 2002;18:262-6.
- [CrossRef] [PubMed] [Google Scholar]
- The potential toxicity of ozone: Side effects and contraindications of ozonetherapy In: Ozone: A new medical drug. Berlin: Springer; 2011. p. :75-84.
- [CrossRef] [Google Scholar]
- Ozone: A possible cause of hemolytic anemia in glucose-6-phosphate dehydrogenase deficient individuals. J Toxicol Environ Health. 1977;2:709-12.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperthyroidism increases the risk of ozone-induced lung toxicity in rats. Toxicol Appl Pharmacol. 2001;173:18-26.
- [CrossRef] [PubMed] [Google Scholar]






