Translate this page into:
Silver diamine fluoride – A review
*Corresponding author: M. Kruthika, Associate Professor, Department of Pedodontics and Preventive Dentistry, Vinayaka Mission’s Sankarachariyar Dental College, Vinayaka Mission’s Research Foundation ( Deemed to be University) Salem, Tamil Nadu, India. smilekruthika@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rajakumari TN, Thiruvenkadam G, Vinola D, Kruthika M. Silver diamine fluoride – A review. J Academy Dent Educ 2020;6(1 & 2):5-10.
Abstract
Untreated dental caries remains a challenge in young children and adolescents. Invasive treatments in very young children and children with special health care needs require advanced pharmacological behaviour management strategies. A minimally invasive treatment modality to arrest caries is by application of 38% Silver Diamine Fluoride (SDF). Besides its efficacy to arrest decay, SDF is favoured by its inexpensiveness. This review enlightens the evolution, historical background, mechanism of action, clinical considerations, advantages and disadvantages of Silver Diamine Fluoride.
Keywords
Silver diamine fluoride
Early childhood caries
Topical fluoride
INTRODUCTION
Dental caries is one of the widespread diseases of stomatognathic system and its prevalence ranges from 49% to 83% across different countries.[1] Various data suggest that there has been a drop globally but still at significantly different rates in high- and middle-/low-income countries. The use of fluorides and established preventive programs were attributed to the declining rates in high-income countries. In low- and middle-income countries, there decline has been less or contrary because of the increasing consumption of sugars and refined foods.[2] According to a national survey conducted in India, the prevalence of dental caries in children aged 5 years was 50%; 52.5% in 12 years old; 61.4% in 15 years old; 79.2% in 35–44 years old; and 84.7% in 65–74 years old.[3] Early childhood caries (ECC) is one of the most commonly uncared disease affecting infants and young children. In India, the prevalence of ECC was found to be 44% among 8–48 months olds, and in rural South India, the prevalence was 40.6% among 0–3-year-old children.[4]
With increased knowledge and understanding of the carious process, the treatment for dental caries takes a paradigm shift from surgical removal of tooth structure to prevention of its occurrence and inhibition of its progression.[5] Conventionally, the management of dental caries has been excavation and drilling to remove the infected and affected portions of teeth which requires skills and creates noise which will be a major downfall while treating pediatric patients. Most of the children affected are young, anxious, and from low socioeconomic families less invasive procedures must be considered to combat the progression of ECC disease process.[6]
A minimal invasive and more bearable treatment is done using 38% silver diamine fluoride (SDF) which can be used in the management of dental caries. It certainly has an advantage of more ease in psychological management of the children and no demand of local anesthesia or no drilling or use of rubber dam and has additional benefits of avoiding anxiety and being economical.[7] The metal silver has become uncovered to the world as early as 4000 BC by Caldeans[8] During 980 AD, Avienna brought silver nitrate to medical attention using it as a blood purifier. However, in early 1600s, many scientists and doctors utilized silver nitrate as purgative, counter irritant and for the therapy of brain infections.[9] However, the first use of silver nitrate in dentistry was in 1840. Later in 1917, ammoniacal solution of silver nitrate has been used for its antimicrobial property and their ability to penetrate dentin.[10] In Japan, silver fluoride is used for a millennium, to which amine was added 80 years ago and used for treating carious lesions[11] and it was approved as cariostatic agent by Central Pharmaceutical Council of Ministry of Health and Welfare and marketed with a trade name of Saforide.[12]
SDF is approved and being used for the past 80 years. On August 2014 in the USA, Food and Drug Administration stated it as Class II medical device. This perceived SDF as a “drug to treat serious or life-threatening conditions” and declares that “exploratory clinical evidence of SDF indicates that it may validate a valuable improvement over existing therapies.”[13] This strikes SDF as a pioneer to substantially state that oral disease is being designated as a serious medical state and promoted its significance in health welfare issues.
HISTORY AND EVOLUTION
In 1969, SDF was first scrutinized by a Japanese scientist Mizuho Nishuro at Osaka University. She explored it to know about the amalgamated effects of silver and fluoride which are known for their antimicrobial and remineralization properties, respectively.[14] In 1970, Western Australia School of Dental Service used a new approach called “two step metal fluoride” by application of silver fluoride and stannous fluoride to prevent new carious lesions.[14] Initially, 10–12% concentration of SDF was explored to know about their effects but they proved to be less effective than 38% SDF.[15]
Several researches are being done by merging different materials in different concentrations such as use of 40% SDF and 10% stannous fluoride and another research with the use of 25% silver fluoride and 5% silver fluoride varnish. However, their beneficial effects evinced to be less effective or similar to that of 38% SDF.[16]
| S. No. | Year | Authors | Conclusion |
|---|---|---|---|
| 1. | 1974 | Suzuki et al.[17] | After 3 min application, fluoride penetrates the enamel of about 25 µ depth and silver penetrates about 20 µ depth |
| 2. | 1994 | McDonald and Sheiham[18] | Caries progression is less in SDF/SnF2groupwhen compared to (i) SnF2group, (ii) SnF2/SDFgroup with minimal cavity preparation, (iii) minimal cavity preparation restored with composite resin, and (iv) no treatment |
| 3. | 1996 | Gotjamanos[19] | About 40% silver fluoride application to residual caries followed by restoration with glass ionomer cement showed a favorable pulpal response |
| 4. | 1999 | Klein et al.[20] | Lesions treated with a single silver fluoride/stannous fluoride or silver nitrate application demonstrated 29% and 19% less lesion progression, respectively. SDF and chlorhexidine did not differ significantly from the control |
| 5. | 2002 | Chu et al.[21] | SDF was found to be effective in arresting dentin caries in primary anterior teeth in pre-schoolchildren |
| 6. | 2005 | Llodra et al.[22] | The mean incidence of dental caries in primary teeth was less in SDF group than in controls. The silver diamine fluoride solution was found to be more effective for caries reduction in school children |
| 7. | 2009 | Yee et al.[23] | Arresting dental caries by treating with 38% SDF provides an alternative modality when restorative treatment for primary teeth is not an option |
| 8. | 2009 | Braga et al.[14] | SDF showed significantly greater effectiveness for arresting carious lesion than glass ionomer sealant and cross tooth brushing technique at 3 and 6 months interval. No differences were observed among the three groups at 18- and 30-month evaluations |
| 9. | 2011 | Lou et al.[24] | SDF appeared to produce globular particles of calcium fluoride on the surface of the hydroxyapatite crystals, which disappeared on washing. SDF reacts with gelatin and particles of silver that were produced were resistant to washing |
| 10. | 2012 | Zhi et al.[25] | Once a year application of either silver diamine fluoride or high fluoride releasing GIC can arrest active dentinal caries. Increasing the frequency of application of SDF increases the caries arrest rate |
| 11. | 2012 | Monse et al.[26] | One time application of 38% SDF on the occlusal surfaces of permanent first molars of 6–8-year-old children is not an effective method to prevent dentinal caries lesions |
| 12. | 2013 | Mei et al.[27] | 38% SDF inhibits multispecies (Streptococcus mutans, S. sobrinus, Lactobacillus acidophilus, Lactobacillus rhamnosus, and Actinomyces naeslundii) cariogenic biofilm formation on dentin carious lesions and reduces the demineralization process |
| 13. | 2013 | Mei et al.[15] | 38% SDF inhibits dual species (Streptococcus mutansand L. acidophilus) cariogenic biofilm formation on dentin carious lesions and reduces the demineralization process |
| 14. | 2014 | Mei et al.[28] | A highly remineralized zone rich in calcium and phosphate was found on the arrested cavitated dentinal lesion of primary teeth. The collagens were protected from being exposed in arrested lesions |
| 15. | 2014 | Mei et al.[29] | The presence of silver in different concentrations of SDF (38%, 30%, and 12%) had inhibitory effect against both cathepsin D and K which contribute to the collagen degradation in caries progress |
| 16. | 2017 | Contreras et al.[30] |
The literature indicates that SDF is a preventive treatment for dental caries in community settings. At concentrations of 30% and 38%, SDF shows potential as an alternative treatment for caries arrest in both primary and permanent dentition |
| 17. | 2017 | Li et al.[31] | The annual application of SDF or SDF/KI solution is effective in preventing root caries among community-dwelling elders in a fluoridated area |
MECHANISM OF ACTION
SDF has antimicrobial action on bacteria causing caries such as strains of Streptococcus mutans, Actinomyces naeslundii, Lactobacillus acidophilus, and Lactobacillus rhamnosus.[27,28,32] It also acts on organic and inorganic portion of tooth by inhibiting the degeneration and promoting remineralization, respectively [Figure 1]. SDF penetrates enamel of about 25 μ[17] and dentin of about 16–200 μ.[33] SDF arrested lesions of 150 μ thick.[28]
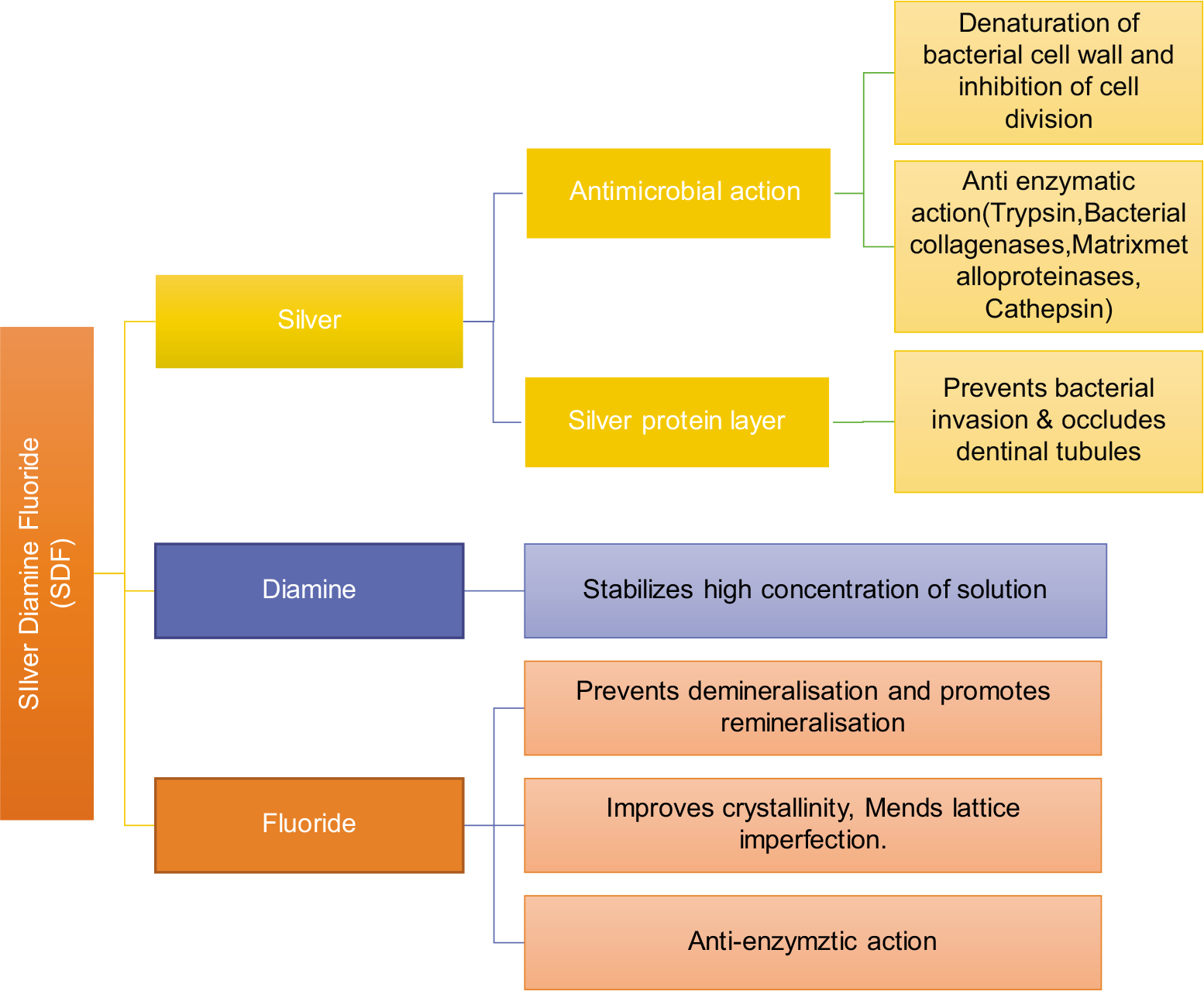
- Flowchart of mechanism of action of silver diamine fluoride.
SDF reacts with hydroxyapatite (HA) crystals (Ca10(PO4)6(OH)2) to form silver phosphate (Ag3PO4) and calcium fluoride (CaF2) as its major byproducts.[21,34]
Ca10(PO4)6(OH)2 + Ag(NH3)2 → CaF2 + Ag3PO4 +NH4OH
SDF can react in the following possible mechanisms:
-
Calcium fluoride is one of the major by-products of the reaction. It reacts with HA to form fluorohydroxyapatite. Fluoride acts on peritubular and intertubular dentin and they improve their resistance against acid decalcification.[35] Fluoride also mends any lattice imperfection[36] and ameliorates their crystallinity,[37] thereby promoting remineralization
Step 1: CaF2 → Ca++ + 2F−
Step 2: Ca10(PO4)6(OH)2 + 2F− → Ca10(PO4)6F2 + 2OH−
The silver phosphate formed in the reaction forms a silver protein layer and obturates the dentinal tubules. This reduces the possibility of bacteria and bacterial byproducts invading into dentin. Researchers also mentioned that SDF has demineralization inhibiting property[29,38]
The antibacterial action of SDF is by its anti-enzymatic activity and dextran-induced agglutination of cariogenic strains of S. mutans. [15] SDF-treated dentin is resistant to trypsin, bacterial collagenase, matix metalloproteinases,[39] and cathepsins[29]
Silver in SDF has its effect on both bacteria and tooth. Silver interacts with sulfhydryl group of proteins, damage to deoxyribonucleic acid, alteration in hydrogen bonding, and inhibits cell wall synthesis and cell division. These effects cause bacterial killing and inhibit biofilm formation[15,32]
Suzuki et al. proposed anti-plaque activity of SDF and stated that they have a minimal inhibitory concentration of 0.12 μ mole/ml against S. mutans and completely inhibits the dextran-induced agglutination of S. mutans at 0.59 μ mole/ml and sucrase activities of S. mutans at 0.2 μ mole/ml. SDF inhibits the adsorption of salivary proteins by HA which prevent plaque formation[17]
Zombie effect:[40] Silver is said to act according to Le Chatelier’s principle. This is because the bacteria that are killed by silver have conspicuous biocidal activity against living bacteria. This is due to the following important characteristics: (i) While killing the bacteria, the metallic silver is not deactivated and (ii) the bacteria that are dead acts as a reservoir for metallic silver and cause sustained release of silver.
Indications
(i) Extreme caries risk patients (salivary dysfunction, secondary to caries treatment, and severe ECC), (ii) due to some medical or psychological conditions such as uncooperative children, elderly patients, physical or cognitive disabilities, and immunocompromised patients, (iii) dentinal hypersensitivity, (iv) vulnerable tooth structures such as exposed roots, (v) difficult to treat carious lesions such as in furcation, (vi) caries prevention in both children and adults, and (vii) difficult to access dental care areas.[7]
Contraindications
(i) Patients who are allergic to silver and (ii) in desquamative conditions such as oral ulcerations, ulcerative gingivitis, or stomatitis.
Advantages
(i) Control of pain and infection, (ii) more economical, (iii) less technique sensitive, and (iv) non-invasive, minimum risk of spreading the infection.
Disadvantages
(i) Darkening of carious lesions (but application of saturated solution of potassium iodide immediately following SDF application is considered to minimize the staining), (ii) temporary tattoo to skin like henna tattoo (which gets resolved in 2–14 days due to skin exfoliation), (iii) stains clothes and clean surfaces, and (iv) patients may experience metallic or bitter taste but the taste response is much better than fluoride varnish.
Case selection for application of SDF
Criteria for selection include
(i) High-risk patients who have active caries lesions, (ii) patients with behavioral problems and medically compromised conditions, (iii) patients with multiple cavitated caries lesions that requires too many visits to dental office, and (iv) patients with lesions that are complicated to treat and with difficulty accessing dental care.[41]
Clinical application of SDF
Step 1: Remove debris from decay cavity to allow better contact with denatured dentin
Step 2: Excavation of carious dentin prior to SDF application is not necessary
Step 3: To avoid tattooing with SDF, a protective coating may be applied to the lips and skin
Step 4: Areas to be treated with SDF should be isolated with cotton rolls or other isolation methods
Step 5: Care should be taken when applying SDF on primary teeth adjacent to permanent anterior teeth that may have non-cavitated (white spot) lesions to avoid inadvertent staining
Step 6: No more than 1 drop of SDF should be used for the entire appointment. One drop (25 μL) is ample material to treat five teeth and contains 9.5 mg SDF
Step 7: Dry the lesion with gentle flow of compressed air
Step 8: Wet the microbrush with SDF and remove excess liquid before application. After application of SDF directly to the affected tooth surface, remove excess to minimize systemic absorption
Step 9: Minimum 1 min application time is necessary
Step 10: Apply gentle flow of compressed air until medicament is dry and keep the area isolated for as long as 3 min.
Safety
The average lethal dose for SDF varies according to the route of exposure, (i) for oral administration –520 mg/kg and (ii) subcutaneous administration – 380 mg/kg.
CONCLUSION
The main advantages of SDF are its low cost, easy availability, and not technique sensitive. It does not require any special instruments or gadgets for application. With proper training, SDF is considered as an ideal material for mass community application to arrest caries at least to underdeveloped and disadvantaged people where there is limited or no access to dental care. In India, it is available in the name of Fagamin (Tedequim, Cordoba, Argentina). Longitudinal studies are expected in this regard to prove its efficacy in arresting dental caries for a prolonged period of time.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global epidemiology of dental caries and severe periodontitis-a comprehensive review. J Clin Periodontol. 2017;44:S94-105.
- [CrossRef] [PubMed] [Google Scholar]
- Declining caries trends: Are we satisfied? Curr Oral Health Rep. 2015;2:212-7.
- [CrossRef] [PubMed] [Google Scholar]
- National Oral Health Survey and Fluoride Mapping, 2002-2003. India: Dental Council of India; 2004.
- [Google Scholar]
- Prevalence and pattern of early childhood caries in a rural South Indian population evaluated by ICDAS with suggestions for enhancement of ICDAS software tool. Int J Pediatr Dent. 2017;27:191-200.
- [CrossRef] [PubMed] [Google Scholar]
- Minimal intervention and concepts for minimally invasive cavity preparations, techniques and materials-a review. J Conserv Dent. 2002;5:101-9.
- [Google Scholar]
- Arresting early childhood caries with silver diamine fluoride-a literature review. Oral Hyg Health. 2013;1:117.
- [CrossRef] [Google Scholar]
- UCSF protocol for caries arrest using silver diamine fluoride: Rationale, indications and consent. J Calif Dent Assoc. 2016;44:16-28.
- [Google Scholar]
- What value has argenti nitras as a therapeutic in dentistry? Int Dent J. 1891;12:661-71.
- [Google Scholar]
- Silver compounds used in dentistry for caries management: A review. J Dent. 2012;40:531-41.
- [CrossRef] [PubMed] [Google Scholar]
- Caries progression in primary molars: 24-month results from a minimal treatment programme. Community Dent Oral Epidemiol. 1981;9:260-5.
- [CrossRef] [PubMed] [Google Scholar]
- Radiographic changes following treatment of dental caries with silver fluoride. . 2019;46:105-12.
- [Google Scholar]
- Silver in health care: Antimicrobial effects and safety in use. Curr Probl Dermatol. 2006;33:17-34.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of silver diamine fluoride on incipient caries lesions in erupting permanent first molars: A pilot study. J Dent Child. 2009;76:28-33.
- [Google Scholar]
- Caries arresting effect of silver diamine fluoride on dentine carious lesion with S. mutans and L. acidophilus dual-species cariogenic biofilm. Med Oral Patol Oral Cir Bucal. 2013;18:824-31.
- [CrossRef] [PubMed] [Google Scholar]
- Paradigm shift in the effective treatment of caries in schoolchildren at risk. Int Dent J. 2012;62:47-51.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of diamine silver fluoride on tooth enamel. J Osaka Univ Dent Sch. 1974;14:61-72.
- [Google Scholar]
- A clinical comparison of non-traumatic methods of treating dental caries. Int Dent J. 1994;44:465-70.
- [Google Scholar]
- Pulp response in primary teeth with deep residual caries treated with silver fluoride and glass ionomer cement (atraumatic technique) Aust Dent J. 1996;41:328-34.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of four anticaries agents on lesion depth progression in an in vitro caries model. Pediatr Dent. 1999;21:176-80.
- [Google Scholar]
- Effectiveness of silver diamine fluoride and sodium fluoride varnish in arresting dentin caries in Chinese preschool children. J Dent Res. 2002;81:767-70.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of silver diamine fluoride for caries reduction in primary teeth and first permanent molars of schoolchildren: 36-month clinical trial. J Dent Res. 2005;84:721-4.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy of silver diamine fluoride for arresting caries treatment. J Dent Res. 2009;88:644-7.
- [CrossRef] [PubMed] [Google Scholar]
- Reaction of silver diamine fluoride with hydroxyapatite and protein. J Dent. 2011;39:612-8.
- [CrossRef] [PubMed] [Google Scholar]
- Randomized clinical trial on effectiveness of silver diamine fluoride and glass ionomer in arresting dentine caries in preschool children. J Dent. 2012;40:962-7.
- [CrossRef] [PubMed] [Google Scholar]
- Caries preventive efficacy of silver diammine fluoride (SDF) and ART sealants in a school-based daily fluoride tooth brushing program in the Philippines. BMC Oral Health. 2012;12:52.
- [CrossRef] [PubMed] [Google Scholar]
- Antibacterial effects of silver diamine fluoride on multi-species cariogenic biofilm on caries. Ann Clin Microbiol Antimicrob. 2013;12:4.
- [CrossRef] [PubMed] [Google Scholar]
- An ex vivo study of arrested primary teeth caries with silver diamine fluoride therapy. J Dent. 2014;42:395-402.
- [CrossRef] [PubMed] [Google Scholar]
- The inhibitory effects of silver diamine fluorides on cysteine cathepsins. J Dent. 2014;42:329-35.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness of silver diamine fluoride in caries prevention and arrest: A systematic literature review. Gen Dent. 2017;65:22-9.
- [Google Scholar]
- Randomized clinical trial on preventing root caries among community-dwelling elders. JDR Clin Trans Res. 2017;2:66-72.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of silver diamine fluoride on dentine carious lesions induced by Streptococcus mutans and Actinomyces naeslundii biofilms. Int J Paediatr Dent. 2012;22:2-10.
- [CrossRef] [PubMed] [Google Scholar]
- Micro-hardness of dentin in primary teeth after topical fluoride applications. J Dent. 2008;36:387-91.
- [CrossRef] [PubMed] [Google Scholar]
- Diamine silver fluoride and its clinical application. J Osaka Univ Dent Sch. 1972;12:1-20.
- [Google Scholar]
- Ultrastructural changes in human dentine exposed to a weak acid. Arch Oral Biol. 1968;13:719-34.
- [CrossRef] [Google Scholar]
- X-ray diffraction studies on effect of fluoride on restoration of lattice imperfections of apatite crystals. J Osaka Univ Dent Soc. 1970;15:42-56.
- [Google Scholar]
- Effects of fluoride on crystallinity of synthetic and biological apatite. J Osaka Univ Dent Soc. 1967;12:95-110.
- [Google Scholar]
- Mechanisms of action of diammine silver fluoride and its use. Nippon Dent Rev. 1970;328:180-7.
- [Google Scholar]
- The inhibitory effects of silver diamine fluoride at different concentrations on matrix metalloproteinases. Dent Mater. 2012;28:903-8.
- [CrossRef] [PubMed] [Google Scholar]
- Antibacterial activity of silver-killed Bacteria: The Zombies effect. Sci Rep. 2015;5:9555.
- [CrossRef] [PubMed] [Google Scholar]
- Chairside guide: Silver diamine fluoride in the management of dental caries lesions. Pediatr Dent. 2017;39:478-9.
- [Google Scholar]






