Translate this page into:
Saliva- A Tool for Diagnosis in Periodontal Disease
*Author for correspondence
-
Received: ,
Accepted: ,
This article was originally published by Informatics Publishing and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Periodontitis, a chronic inflammatory condition involving tooth supporting structures that results in connective tissue loss and progressive bone loss. Careful diagnosis and treatment plan is inevitable for the successful clinical outcome. Investigation of biomarkers specific to certain periodontal disease in saliva gains more clinical interest in the present era. The gratification towards saliva has been increased over GCF due to its ease and non-invasive methods of collection compared to GCF. Saliva contains numerous biomarkers which is an emerging chair side diagnostic tool that will play a major role for the future investigators. This article aims at reviewing the biomarkers present in the saliva pertaining to particular periodontal diseases and its activity.
Keywords
Periodontitis
Salivary Biomarkers
Salivary Enzymes
1. Introduction
Successful periodontal therapy relays on early diagnosis and severity of a disease1. Periodontitis, which is a most common periodontal disease category, is a irreversible inflammatory chronic condition that persuades to formation of probing pocket depth, progressive attachment loss, with loss of collagen fibres and can progress to bone loss if left untreated2. Traditional diagnostic parameters fails to assess patients who are highly susceptible to periodontitis. The diagnostic use of saliva has attracted the attention of clinical investigators due to its non-invasiveness and ease of collection.
2. Emerging Diagnostic Tool-Saliva
Saliva plays a major role in lubrication, chewing, swallowing, digestion and protection of oral mucosa4. Local and general health of the human body is reflected as an essential biomarker in the saliva. Although gingival crevicular fluid plays a potential role in early diagnosis of periodontal disease progression3, the invasive and complex collecting procedure offers a technical challenge to the clinician.
3. Gratification of Saliva over Gingival Crevicular Fluid5
Painless collection process
Less distress to patient
Simple to collect and non-invasive
Convenient for multi sampling
Cost effective for screening large population
Cheap technology for laboratorial diagnosis
Easy to store
Less time consuming
Less blood contamination
4. Salivary Biomarkers in Periodontal Diseases
A biomarker is a substance used as an indicator for early disease detection and disease progression in diagnosis of oral diseases6. The bacterial products released during periodontal disease progression activate the immune response and triggers the various inflammatory cells such as polymorphonuclear neutrophils, monocytes, macrophages. Thus resulting in the release of various cytokines (prostaglandin E2, tumor necrosis factor and interleukins) and inflammatory markers in serum and saliva. Consequently the release of matrix metalloproteinases and collagen destructive enzymes leads to the extra cellular matrix degradation, a trespasser for periodontal disease progression.
The various salivary biomarkers2 includes
-
Markers affecting dental biofilm
Specific marker
Non specific
Systemicbiomarkers to periodontal infection
Markers of periodontal soft tissue inflammation
Markers of alveolar bone loss
Salivary enzymes and ions
Growth factor as a salivary biomarker
Epithelial keratins
Hormones
Inflammatory cells and bacteria
Volatiles and oxidative stress marker
4.1 Markers Affecting Dental Biofilm
4.1.1 Specific Marker
Immunoglobulin interferes in adherence of bacterial metabolism in chronic and aggressive periodontitis. Increased concentration of immunoglobulin in patients with periodontitis has been clinically evident. Higher salivary constituents of various immunoglobulins such as IgA, IgG, IgM specific to certain periodontal pathogens are observed as a salivary parameter in patients with periodontitis compared to Non-periodontitis individuals. Especially, level of IgA has been greatly detected and their levels decreased significantly following non-surgical periodontal therapy.
4.1.2 Non Specific Biomarker (Table 1)
| Protein Markers | Nature of the Biomarker | Mechanism | Activity in Periodontitis |
|---|---|---|---|
| Mucins7 | Glycoproteins(MG1,MG2) helps in maintaining the viscoelasticity of saliva | Interferes with attachment of A. actinomycetemcomitans | MG2 level declined in saliva with increased periodontal pathogens |
| Lactoferrin2,7 | Iron binding glycoprotein | Inhibit the growth of bacterial by lowering the iron content | i)Upregulated in gingival inflammation ii)Higher concentration in periodontal disease |
| Histatin2,7 | Salivary protein with antimicrobial properties | i) Neutralizes enzymes and lipopolysaccharides in gram negative bacteria ii) Inhibits the histamine expressed |
Decreases the role of histamine |
| Fibronectin7 | Glycoprotein | Improves the attachment and colonisation of bacteria | Additive role in repair and healing process |
| Cystatins7 | Proteolytic enzyme released by bacteria inflammatory cells, osteoclast, fibroblast | Collagenolytic activity causing tissue destruction | Modulating enzyme activity in periodontium |
| Platelet Activating Factor (PAF)7 | Stimulates the phospholipid and triggers the inflammation | Release of inflammatory mediators | Positive correlation between PAF and periodontal inflammation |
| Proline7 | Amino acid | Degradation of amino acid | Both positive and negative correlation exist |
4.2 Systemic Biomarker - C-Reactive Protein
Periodontal inflammation causes stimulation of circulatory cytokines such as tumour necrosis factor α, interleukin-1 which inturn induces the liver to produce C-reactive protein into the circulation. Salivary C-reactive protein is appreciated in chronic and aggressive periodontitis and act as inflammatory marker2.
4.3 Markers Present in Inflamed Periodontium
Prostaglandin E2 is the major mediator of periodontal disease and act as a potent biomarker of soft tissue inflammation (figure 1). PGE2 stimulates the fibroblast and osteoblast to produce MMP’S which is again a potential biomarker of tissue destruction2.
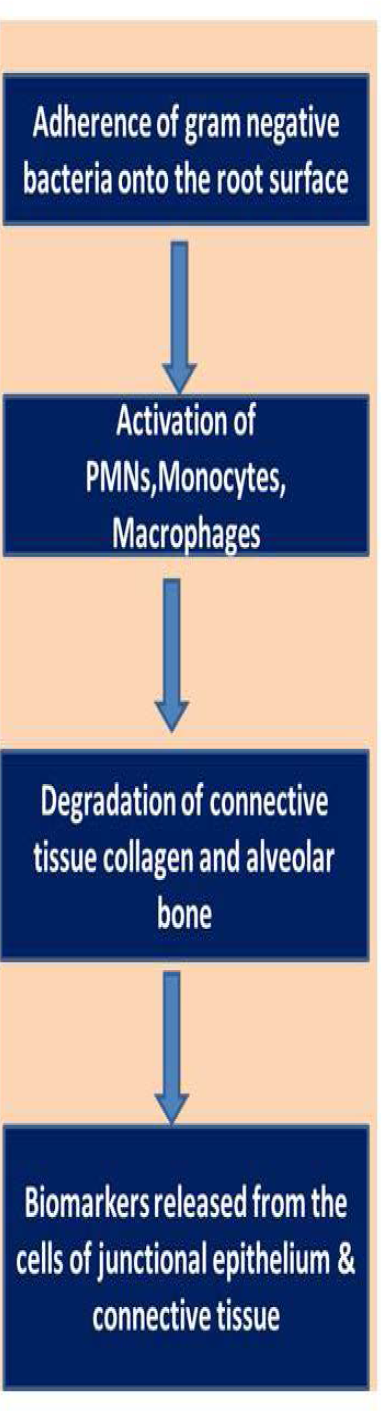
- Mechanism of biomarker release due to soft tissue inflammation.
4.4 Markers Expressed in Alveolar Bone Loss
MMPs are responsible for tissue destruction and remodelling. Periodontal collagens are broken down by collagenases. MMP8 levels are most prevalent in active disease progression of patients with gingivitis and periodontitis. Also in patient with peri-implantitis the peri-implant sulcular fluid demonstrates an elevated level of MMP8. The need for future longitudinal studies in the salivary level of MMP8 in periodontitis patient is inevitable2,7.
Gelatinase (MMP9) is a collagenase produced by neutrophils and has a pivotal role in degradation of collagenous intercellular ground substance. MMP9 increased in patients with periodontitis has been reported in the literature by Teng et al8.
Collagenase (MMP13) is another collagenolytic MMP found to be elevated in patients with periodontitis and peri-implantitis7.
Increase in concentration of telopeptide, osteocalcin, osteopontin in GCF of patients with progressive periodontal disease has been reported7.
4.5 Salivary Enzymes and Ions
The major salivary enzymes which act as potential biomarkers include lysozyme and peroxidase. Lysozymes are capable of breaking chemical bond in bacterial cell wall and hydrolyze the glycosidic linkages and distrupts the bacterial cell wall. Low level salivary lysozyme with high level of salivary peroxidase is considered as a factor for periodontal disease7.
Increased salivary calcium demonstrated in the saliva of patient with periodontal disease has been reported in the literature by Sewon et al9.
4.6 Growth Factor as a Salivary Biomarker
Growth factor act as remarkable biomarker in inflammation and wound healing. Higher levels of growth factor were detected in whole saliva of patient with periodontitis7.
4.7 Epithelial Keratins
Morgan et al., demonstrated the epithelial cells lining the mucosa can be demonstrated in patients saliva with periodontitis10.
4.8 Hormones
High salivary cortisol level has been demonstrated in patients with periodontitis along with emotional stress, poor oral hygiene, smoking7.
4.9 Inflammatory Cells and Bacteria
Increased orogranulocytic migration rate in the presence of oral inflammation has been reported by Raeste et al11. Klinkhammer et al., developed the orogranulocytic migration rate12.
Asikainen et al., Umeda et al., demonstrated the presence of microorganisms in the whole saliva13. Dejong et al., concluded saliva as a culture medium for Streptococcus and Actinomyces in his study14.
4.10 Volatiles and Oxidative Stress Marker
Hydrogen peroxide, methyl mercaptans are the known volatile sulphur compounds which act as a diagnostic marker in periodontal disease.
This results due to excessive free radicals or diminished antioxidant system. Oxidative stress leads to DNA damage including oxidation of nucleosides (8-hydroxy deoxy guanosine) which is a potent biomarker of oxidative stress. Biomarkers ellicited in periodontitis has been summarized in (Table 2).
| Authors | Aim | Outcome |
|---|---|---|
| Baltacioglu et al17 | Evaluation of lipid peroxidation(malondialdehyde) level and total oxidant/antioxidant in patients serum and saliva | Salivary MDA level, TOS, TAOS are elevated in periodontitis group than control group |
| Priscila et al18 | Compared the salivary concentration of matrix metalloproteinase 8, interleukin 6,osteoprotegrin in periodontitis patients with or without diabetes | Salivary IL-6 concentration is increased in both the groups while salivary MMP8 and OPG are elevated in patients with diabetes and periodontal inflammation |
| Ghallab et al19 | Investigated the salivary soluble CD44 profiles of smoking and non-smoking patients with and without periodontitis in counter to SRT | Baseline salivary soluble CD44 elevated in smokers compared with non-smoking periodontitis group |
| Gursoy et al20 | Concentration of ICTP, MMP8, MMP14 and TIMP1 were analysed to detect potential markers of periodontitis | MMP8,MMP14,TIMP1 and ICTP are highly susceptible in advanced periodontitis patients |
| Al-Rawi et al21 | Comparison of relationship between resist in and period onto pathogenic bacterial levels in obese adults, obese patients with type 2 diabetes and healthy controls | obese individuals with type 2 diabetes exhibited high level of salivary resist in |
| Nomura et al22 | Evaluated the level of alanine amino transferase,alkaline phosphatase and free haemoglobinas biomarker also the count of P. intermedia, P. gingivalis, T. forsythia in stimulated saliva | Low P. Gingivalis and ALT act as a potential indicator for the progression of periodontal disease |
| Bertl et al23 | Assessed the effect of non surgical periodontal therapy on salivary malotonin levels | Decreased salivary malotinin levels are the baseline which progressively increased at the end of the study |
| Novacovic et al24 | Investigated the impact of nonsurgical periodontal treatment and salivary antioxidants(albumins, uricacid, superoxide dismutase, glutathione peroxidase) and evaluated their capacity as a biomarker | All the clinical parameters except attachment level were remarkably decreased after SRP |
| Ramseier et al25 | Microbially derived biomarkers of plaque biofilm and saliva is determined | MMP-8,9and osteoprotegerin along with red-complex anaerobic bacteria were detected. |
| Miller et al26 | Conducted the study to determine the correspondence between periodontal disease and levels of IL-1ß, MMP8, OPG in saliva of patients with moderate to severe periodontitis | Salivary MMP8 and IL-1ß are visible to serve as biomarker of periodontal disease |
| Banasova et al27 | Compared oxidative stress salivary markers and feature of salivary DNA to the patients with chronic periodontitis and free control groups | Salivary thiobarbiturics acid reacting substances were higher in periodontitis subjects than controls and no differences found regarding salivary DNA |
| Sexton et al28 | Assessed the salivary biomarkers (IL-1ß,IL-8,MIP1α, MMP8, OPG,TNF-α) of periodontitis patients | Salivary biomarker level of IL-1ß, MMP8, OPG and MIP1α reflected the disease severity |
| Tabari et al29 | Evaluated the salivary concentration of visfatin level in patients with chronic periodontitis | Increased concentration of salivary visfatin level were significantly higher in periodontitis group |
| Arroyave et al30 | Determined the difference in salivary concentration of sRANKL, osteoprotegrin and its ratio in periodontal disease | Higher salivary concentration of sRANKL, osteoprotegrin and its ration in periodontitis patients |
| Yesica et al31 | Investigated the salivary levels of 8-hydroxy-2-deoxy guanosine and human neutrophil elastase complex as salivary biomarker in patient with chronic periodontitis | Increased salivary levels 8-hydroxy-2-deoxy guanosine and human neutrophil elastase in chronic periodontitis patient |
5. Forthcoming Biomarker in Saliva for Periodontitis
5.1 Salivary Proteome
A varying group of proteins manifested by a genome or a cell or a tissue or an organism referred as proteome. Mass spectrometry and shot gun proteomics are techniques that are used to identify proteomes2.
5.2 Salivary Transcriptome
Transcriptome refers to an RNA molecules present in a single cell or a group of cells. Li et al., demonstrated the elevated RNA molecules in saliva of patients with oral cancer tissues15.
Zudakov et al., demonstrated the five salivary RNA markers (SPRR1A SPRR3, KRT6A, KRT13, KRT4) lasted till 180days in the saliva and blood samples16.
6. Conclusion
Thus biomarkers which are present in the saliva act as effective diagnostic tool because of its ease of collection, cost and chair side diagnostic tool. But still a lot more research efforts are necessary to determine the sensitivity and specificity of salivary biomarker and to increase the availability of routine detection methods32.
References
- Saliva as a diagnostic tool for oral and systemic disease. J Oral Biol Craniofac Res. 2016;6(1):66-75.
- [CrossRef] [PubMed] [Google Scholar]
- Saliva as a diagnostic tool for periodontal disease: Current state and future directions. Periodontology. 2000-2009;50(1):52-64.
- [CrossRef] [PubMed] [Google Scholar]
- Use of salivary biomarker for diagnosis of periodontal disease activity: A literature review. World Journal of Dentistry. 2013;4(4):250-5.
- [CrossRef] [Google Scholar]
- Saliva diagnostics-current views and directions. Exp Biol Med (Maywood). 2017;242(5):459-72.
- [CrossRef] [PubMed] [Google Scholar]
- Saliva-A diagnostic tool. IOSR Journal of Dental and Medical Sciences. 2013;11(6):96-9.
- [Google Scholar]
- Saliva: A diagnostic biomarker of periodontal disease. J Indian Soc Periodontol. 2011;15(4):310-7.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival crevicular fluid gelatinase and its relationship to periodontaldisease in human subjects. J Periodontal Res. 1992;27(5):544-52.
- [CrossRef] [PubMed] [Google Scholar]
- Calcium and other salivary factors in periodontitis affected subjects prior to treatment. J Clin Periodontol. 1995;22(4):267-70.
- [CrossRef] [PubMed] [Google Scholar]
- Potential applications of anti-keratin antibodies in oral diagnosis. J Oral Pathol. 1987;16(4):212-22.
- [CrossRef] [PubMed] [Google Scholar]
- Rate of migration of oral leukocytesin-patients with periodontitis. Scand J Dent Res. 1978;86(1):43-51.
- [PubMed] [Google Scholar]
- Quantitative evaluation of gingivitis and periodontal disease (I): The orogranulocyte migratory rate Periodontics. . 1968;6(5):207-11.
- [Google Scholar]
- Recovery of A actinomycetemcomitans from teeth, tongue and saliva. J Periodontal. 1991;62(3):203-6.
- [CrossRef] [PubMed] [Google Scholar]
- Growth of oral streptococcus species and actinomycesvicosus in human saliva. App Environ Microbiol. 1984;47(5):901-4.
- [PubMed] [Google Scholar]
- Salivary transcriptome diagnostics for oral cancer detection. Clin Cancer Res. 2004;10(24):8442-50.
- [CrossRef] [PubMed] [Google Scholar]
- Stable RNA markers for identification of blood and saliva stains revealed from whole genome expression analysis of time-wise degraded samples. Int J Legal Med. 2008;122(2):135-42.
- [CrossRef] [PubMed] [Google Scholar]
- Lipid peroxidation levels and total oxidant/antioxidant status in serum and saliva from patients with chronic and aggressive periodontitis. Oxidative stress index: A new biomarker for periodontal disease? J Periodontol. 2014;85(10):1432-41.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary interleukin-6, matrix metalloproteinase-8 and osteoprotegerin in patients with periodontitis and diabetes. J Periodontol. 2010;81(3):384-91.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative evaluation of salivary soluble CD44 levels in periodontal health and disease. Journal of Indian Society of Periodontology. 2014;18(6):734.
- [Google Scholar]
- Salivary MMP-8, TMP-1, and ICTP as markers of advanced periodontitis. J Clin Periodontal. 2010;37(6):487-93.
- [CrossRef] [PubMed] [Google Scholar]
- The relation between periodontopathogenic bacterial levels and resistin in the saliva of obese type 2 diabetic patients. Journal of Diabetes Research 2017
- [CrossRef] [PubMed] [Google Scholar]
- Salivary biomarkers for predicting the progression of chronic periodontitis. Archives of Oral Biology. 2012;57(4):413-20.
- [CrossRef] [PubMed] [Google Scholar]
- Non-surgical periodontal therapy influences salivary melatonin levels. Clinical Oral Investigations. 2013;17(4):1219-25.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary antioxidants as periodontal biomarkers in evaluation of tissue status and treatment outcome. J Periodont Res. 2014;49(1):129-36.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of pathogen and host-response markers correlated with periodontal disease. J Periodontol. 2009;80(3):436-46.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary biomarkers of existing periodontal disease: A cross-sectional study. J Am Dent Assoc. 2006;137(3):322-9.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary DNA and markers of oxidative stress in patients with chronic periodontitis. Clinical Oral Investigations. 2015;19(2):201-7.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary biomarkers of periodontal disease in response to treatment. J Clin Periodontol. 2011;38(5):434-41.
- [CrossRef] [Google Scholar]
- Salivary visfatin concentrations in patients with chronic periodontitis. J Periodontol. 2014;85(8):1081-5.
- [CrossRef] [PubMed] [Google Scholar]
- Association of salivary levels of the bone remodelling regulators sRANKL and OPG with periodontal clinical status. J Clin Periodontol. 2012;39(12):1132-40.
- [CrossRef] [Google Scholar]
- Prognostic Value of 8-Hydroxy-2'-Deoxyguanosine and Human Neutrophil Elastase/α1-Proteinase Inhibitor Complex as Salivary Biomarkers of Oxidative Stress in Chronic Periodontitis. Journal of periodontology. 2015;86(11):1260-7.
- [CrossRef] [Google Scholar]
- Salivary markers for periodontal and general disease. Disease Markers 2016
- [CrossRef] [PubMed] [Google Scholar]






