Translate this page into:
Incidence of complications after the surgical removal of impacted mandibular third molars: A single center retrospective study
-
Received: ,
Accepted: ,
How to cite this article: Prerana G, Tantry D, Sougata K, Sivalanka SC. Incidence of complications after the surgical removal of impacted mandibular third molars: A single centre retrospective study. J Acad Dent Educ 2021;7(1):10-7.
Abstract
Objectives:
The aim of the study was to study the incidence of complications associated with the surgical removal of impacted mandibular third molars in a single center.
Material and Methods:
A single center retrospective study was conducted in the Department of Oral and Maxillofacial Surgery at NSVK Sri Venkateshwara Dental College and Hospital located in Bannerughatta, Bengaluru. The study included patients between the ages of 15–60 years who had undergone surgical extraction of one or more mandibular third molar and had a difficulty score between 3 and 6 (Pederson’s difficulty index). During the course of study variables such as age, gender, impacted side, difficulty index, medical, and habit history along with complications and medications were recorded and accessed from the patient’s case history reports. In due course of the study, these variables were analyzed and correlated using descriptive analysis, Chi-square test, Contingency test, and regression analysis to understand whether or not these variables play an important role in aggravating post-extraction complications for mandibular third molars.
Results:
The study sample was composed of 250 patients with 52% female and 48% male with a mean age of 34 years. The complication rate observed was 7.6%, there was a statistically significant co-relation seen between gender (P = 0.016), age groups (p<0.05), spatial relationship (P = 0.019), and medical history (P = 0.016) when compared to the complications observed. The most common complications observed were trismus/muscle spasm followed by dry socket. However, the cases of neurosensory complications were extremely rare.
Conclusion:
There was a significant association to be found between the complication-rate and gender. Conditions such as muscle spasms/trismus and dry socket had a significant predilection toward the males while complications associated with neurosensory changes were commonly seen in females. There was also a significant association between habit history and rate of complication especially in conditions such as dry-socket where all the observed cases had positive history of tobacco/pan chewing habit. Interestingly all the males who complained of dry socket also had reported medical history of type (2) diabetes. Patients with complications such as neurosensory changes were few and could have been prevented with good surgical skills and precision; moreover, even if they were found they were temporary and treated with regular follow-ups.
Keywords
Complications
Third molar
Impaction
Surgical extraction
INTRODUCTION
It has been estimated that the prevalence of third molar impaction is somewhere between 16.7% and 68.3%[1] of which mandibular third molars occupy a majority of around 58.76% of the cases.[2,3] The median age for the eruption of these also commonly referred to as the “Wisdom tooth” is somewhere between the ages 17–23 years.[4] However, it has been seen in most of the studies that mandibular third molar fail to erupt in the oral cavity while remaining significantly impacted. Surgical removal of these molars is one of the most common surgical procedures carried out. In simple words, an impaction is a pathological situation where the tooth fails to erupt in the dental arch during its developmental time and is thereby retained. In many cases these impacted tooth show no signs or symptoms; however, during other times, the patient can present with conditions such as pericoronitis with a probability of facial space infection, periodontal problems in relation to the second molars, fibrosis, trismus, etc. In such conditions, it is but imperative for the clinician to opt in for surgical removal of these impacted teeth. However, it is to be understood that these third molar surgeries can lead to serious complication such as dry socket (alveolar osteitis), pain and swelling, inflammation, dento-alveolar fracture, paraesthesia of the inferior alveolar nerve, or sometimes even lingual nerve damage. It has been estimated that the accident or the complication rate involved in these surgical procedures can vary anywhere between 2.6 and 30.9%.[4,5] The huge variation in the data underlines the fact that these complications arise from a number of factors such as age, health, gender, difficulty level of the impaction, surgeon’s experience, and previous habit histories[6] as well such as smoking.
The purpose of this study is to understand the various complications associated with mandibular third molar impaction and to study whether or not these complications are associated with any variables included in the study such as age, gender, difficulty index, habit and systemic history, and medications involved. The significance of this study is that, a number of factors can have an influence on the outcome of the procedure, thus studying those factors help us to develop skills to avoid or reduce the incidence of the complications.
MATERIAL AND METHODS
Sample design
To address our study objective, we designed a retrospective cohort study. The study sample was chosen among the cohort of patients treated by the surgeons at the Department of Oral and Maxillofacial Surgery, Sri Venkateshwara Dental College and Hospital between January 2016 and February 2020. Baseline data were obtained from patient data bases which had been reported as a part of routine case history discussions. 250 patients were included for the study all of whom met the inclusion criteria.
Inclusion criteria
The patients included in the study were aged between 15 and 60 years all of whom had undergone the surgical extraction of one or more impacted mandibular third molar with the difficulty score within the range of 3–6 according to Pedersons’s difficulty index. Post the surgical extraction procedure these patients were further analyzed for their follow-up appointments to obtain evidences about their post-operative healing.
| Pederson’s difficulty index | |
|---|---|
| Classification | Value |
| Spatial relationship a. Mesioangular b. Horizontal/transverse c. Vertical d. Distoangular |
a. 1 b. 2 c. 3 d. 4 |
| Depth a. Level a: high occlusal level b. Level b: medium occlusal level c. Level c: low occlusal level |
a. 1 b. 2 c. 3 |
| Ramus relationship a. Class 1: sufficient space b. Class 2: reduced space c. Class 3: no space |
a. 1 b. 2 c. 3 |
| Difficulty index a. Very difficult b. Moderately difficult c. Slightly difficult |
a. 7-10 b. 5-6 c. 3-4 |
Exclusion criteria
All the patients below the age of 15 years and above the age of 60 years, and those who had a difficulty score of 6 or more according to Pederson’s difficulty index were excluded from the study.
Study design
The demographic details were noted as a part of routine case history documentation during their visit to the Department of Oral and Maxillofacial Surgery. Symptomatic patients were given prophylactic antibiotics and analgesics before carrying out the surgery. The surgical procedures were performed under aseptic conditions.
All the extractions were carried out after the administration of suitable nerve blocks with Local anesthesia containing 2% Lignocaine HCl with 1:80,000 adrenaline. After the administration of Local anesthesia, a number 15 Bard Parker blade was used for incision. A modified Ward’s incision was used to raise full thickness mucoperiosteal flap. The flap was elevated using Molt’s No.9 periosteal elevator and Howarth’s periosteal elevator. Bone removal was done using surgical drills, elevators and/or forceps. Tooth sectioning was carried out wherever necessary depending on the difficulty level of the case. After tooth extraction, the sockets were irrigated with Povidine iodine, bony irregularities were thoroughly filed. Surgical wounds were closed using 3–0 Black Braided Silk Non-Absorbable sutures. Following the procedure, detailed post-operative instructions were given to the patients and suitable antibiotics and analgesics were prescribed. Routine follow-up was done for 3 weeks. All the patients with post-operative complications were treated and assessed along with regular follow-ups.
Variables
The variables included in the study were age, gender, side of impaction, type of impaction, and difficulty level according to PEDERSON’s classification and the systemic medical history of the patient. Other factors such as habit history of the patient and prophylactic antibiotics administration were also recorded.
Demographic base line data of age and gender were all obtained as mentioned from case history recordings. Post the examination and noting the side of impaction the patients were advised OPG which allowed for the angulation assessment on basis of Winter’s classification (mesioangular, vertical, horizontal, and Distoangular). It also provided sufficient data to comply with other variables such as Depth of impaction- Pell and Gregory classification (Level I, Level II, and Level III) and Position classification (Positions A, B, and C). Other variables such as habit history were noted during the case history discussions on basis of the frequency. There were also some patients who presented with systemic complications such as type (2) diabetes, asthma, hypertension, and thyroid disorders. All of these patients were asked to obtain consent from physicians before the procedure and patients with type 2 diabetes were also advised to undergo routine examinations such as Fasting Blood Sugar tests and Random Blood Sugar tests before performing the procedure.
Once the patients came for routine follow-ups, the site of surgery was examined for healing or presenting complications such as trismus, dry socket, lingual nerve damage, inferior alveolar nerve damage, and infection. Trismus was defined as mouth opening less than 10 mm measured in correlation to the incisal edges of the upper and lower incisal edges,[7] dry socket was examined for signs and symptoms such as severe pain which could not be controlled with analgesics post 3 days of surgery and empty foul smelling socket with loss of primary sutures.[8] Nerve damage was examined as any neurosensory change observed subjectively in the patient through touch or prick performed by the investigators.[9] Infection and swelling were examined as localized tender swelling in the operated area with discharge occurring 3–5 days post-surgery.[9] All these variables were carefully examined and noted to produce results for the study.
Once all the data was received that the data were analyzed using SPSS software using descriptive analysis and Chi-square test, contingency tests, and co-relation analysis to obtain relationship between the variables and complications.
RESULTS
A total of 250 (n = 250) subjects were included for the study, who had undergone the extraction of one or more mandibular third molar between the time period of January 2016–February 2020. Out of 250 subjects included for the study 130 (52%) female patients and 120 (48%) male patients [Figure 1].
Age of the subjects ranged from 15 to 60 years with the mean age being 34 years. Majority of the patients were in the age group of 20 to 29 years (38.4%), followed by 30–39 years (32.4%) age group [Figure 2].
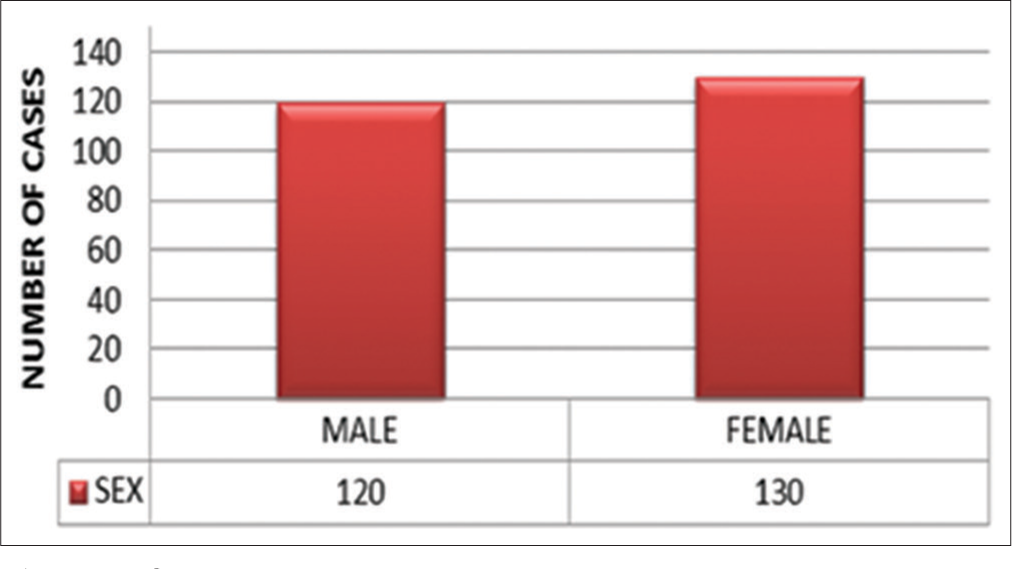
- Sex
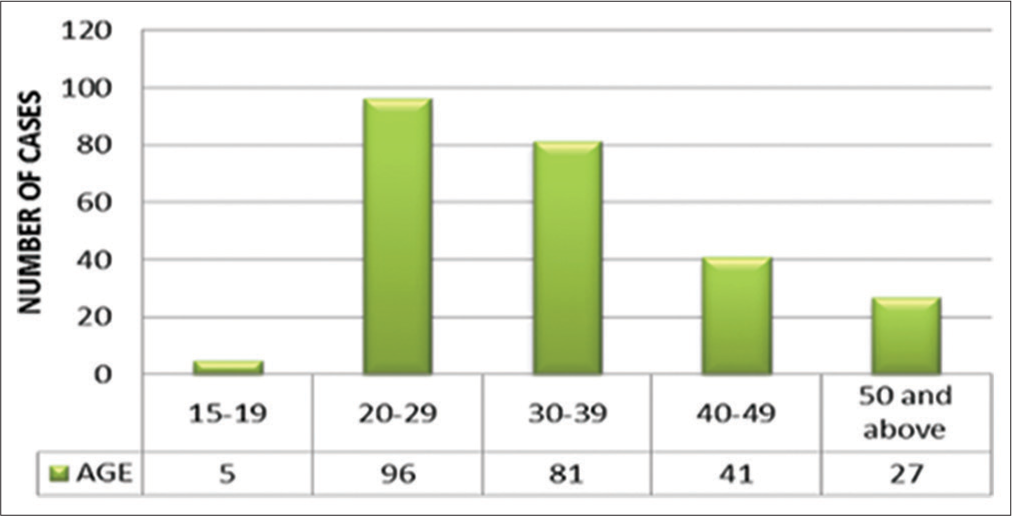
- Age
126 cases, that is, (51.4%) presented with an impaction in the left mandibular third molar, whereas 124 cases, that is, (48.6%) presented with impaction in the right mandibular third molar [Figure 3].
121 out of 250 cases of impaction turned out to be mesioangular type, accounting for 48.4% of total number of cases; this was followed by Distoangular type of impaction in 76 (30.4%) patients. Vertical impaction was seen in 30 (12%) patients. Horizontal impaction was seen only in 23 (9.2%) patients making it the least common type in our study [Figure 4].
The difficulty levels of the cases were assessed based on difficulty index for the removal of mandibular 3rd molar described by Pederson. Accordingly, all the cases were grouped into slightly difficult and moderately difficult. About 59.2% of all the cases were moderately difficult (score between 5 and 6) and 40.8% of all the cases were slightly difficult (score between 3 and 4) [Figure 5].
Many patients presented with systemic conditions, of which history of type (2) diabetes was recorded in 25(10%) patients. History of hypertension was presented by 14 (5.6%) patients. This was followed by thyroid disorders including both hypothyroidism and hyperthyroidism in 6 (2.4%) patients. Six (2.4%) patients presented with the history of asthma and 3 (1.2%) patients presented with the history of epilepsy [Figure 6].
Few patients presented to the department with the history of adverse habits which included Tobacco chewing, Paan /Gutka chewing, areca nut chewing and alcoholism
The overall complication rate was observed to be 7.6% of the total sample population including intra-operative and post-operative complications [Figure 7]
A correlation was established between the complications and age [Table 1], gender [Table 2], spatial relationship [Table 3], and depth of impaction [Table 4] as indicated
Statistically, there was significant relation between complications observed in the follow-up cases and variables such as gender (P = 0.016), age groups (P < 0.05), spatial relationship (P = 0.019), and medical history (P = 0.016).
Muscle spasm was the most common post-operative complication to be seen. About 2.4% of the total sample population which included five male patients and one female patient reported back to the department with limited ability to open mouth. All six patients were above the age of 25. All of these six patients had either Distoangular impaction or vertical type of impaction with a difficulty score between the ranges of 5 and 6.
Patients who reported back to the department with the complaint of Dry Socket after the surgical extraction were all males. Three out of four of them had a positive history of diabetes and had presented with a positive habit history of tobacco smoking. All the four patients were above the age 40 years, with the youngest being 41 years and the oldest patient being 47 years. All of them had vertical type of impaction with difficulty scores in the range of 5–6.
Temporary neurosensory changes were observed mostly in women (0.8%) who were above the age of 30 years. They did not have any significant medical history or habit history. One out of these two patients had a distoangular type of impaction with the difficulty score of 6 and other patient had a vertical type of impaction with a difficulty score of 5.
The two patients who complained of post-operative bleeding were both females above the age of 45 years. Out of them, one patient had a history of hypertension. There was no relevant habit history in both the patients. The female patient with hypertension had a vertical type of impaction with difficulty score of 5; the other patient had a distoangular type of impaction with a difficulty score of 6.
Intra-operative complications were encountered during the procedure which most commonly involved fracture of the root tip in 3 (1.2%) patients. The 3 (1.2%) patients had a distoangular type of impaction with a difficulty score of 6 and were in the ages between 35 years and 39 years. Profuse bleeding occurred in 2 (0.8%) patients, both females above the age of 40 years with no systemic/ habit history.

- Side

- Type of impaction
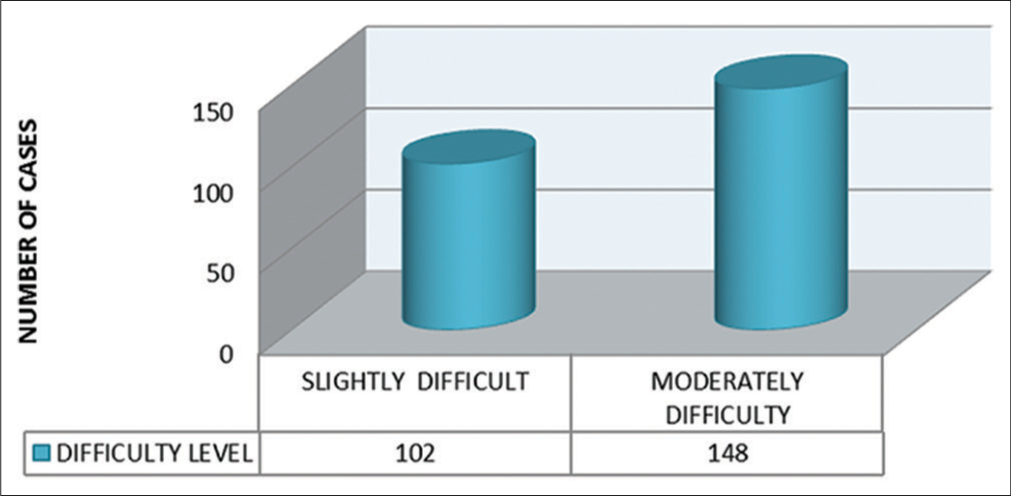
- Difficulty level

- Systemic history
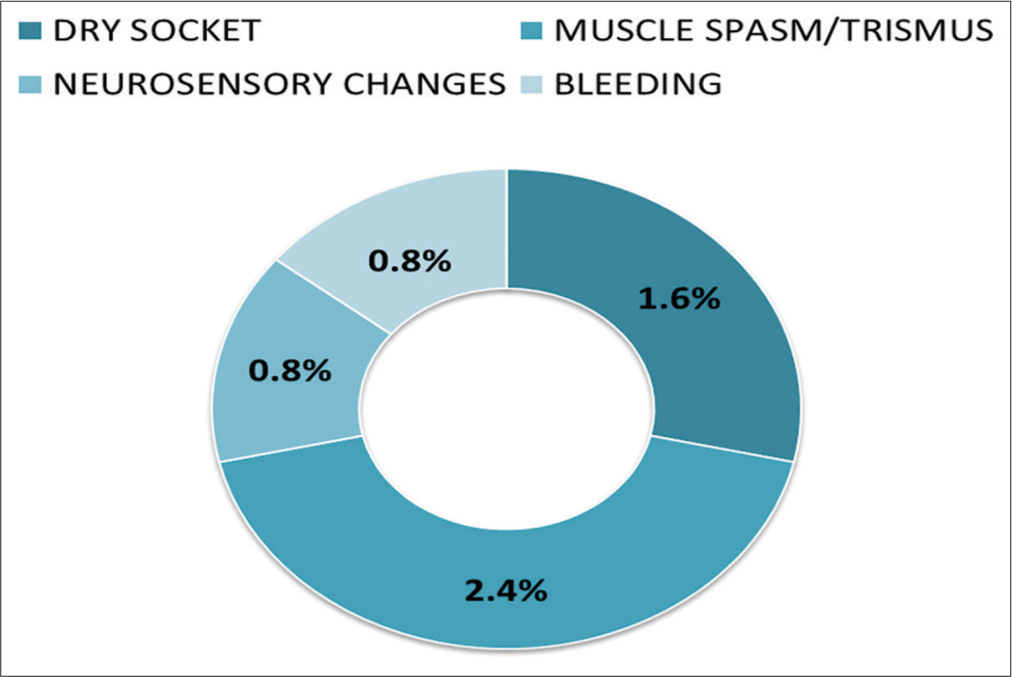
- Post extraction complications
| Age | Frequency | |
|---|---|---|
| Bleeding | 21–30 | 0 |
| 31–40 | 0 | |
| 41–50 | 2 | |
| Total | 2 | |
| Dry socket | 21–30 | 0 |
| 31–40 | 0 | |
| 41–50 | 4 | |
| Total | 4 | |
| Muscle spasm | 21–30 | 3 |
| 31–40 | 3 | |
| 41–50 | 0 | |
| Total | 6 | |
| Neurosensory change | 21–30 | 0 |
| 31–40 | 2 | |
| 41–50 | 0 | |
| Total | 2 |
| Gender | Frequency | Percentage | |
|---|---|---|---|
| Bleeding | Female | 2 | 100.000 |
| Male | 0 | 0.000 | |
| Total | 2 | 100.000 | |
| Dry socket | Female | 0 | 0.000 |
| Male | 4 | 100.000 | |
| Total | 4 | 100.000 | |
| Muscle spasm | Female | 1 | 16.667 |
| Male | 5 | 83.333 | |
| Total | 6 | 100.000 | |
| Neurosensory change | Female | 2 | 100.000 |
| Male | 0 | 0.000 | |
| Total | 2 | 100.000 |
| Spatial relationship | Frequency | Percentage | |
|---|---|---|---|
| Bleeding | Distoangular | 1 | 50.000 |
| Vertical | 1 | 50.000 | |
| Missing | 0 | 0.000 | |
| Total | 2 | 100.000 | |
| Dry socket | Distoangular | 0 | 0.000 |
| Vertical | 4 | 100.000 | |
| Missing | 0 | 0.000 | |
| Total | 4 | 100.000 | |
| Muscle spasm | Distoangular | 4 | 66.6600 |
| Vertical | 2 | 33.3700 | |
| Missing | 0 | 0.000 | |
| Total | 6 | 100.000 | |
| Neurosensory change | Distoangular | 1 | 50.000 |
| Vertical | 1 | 50.000 | |
| Missing | 0 | 0.000 | |
| Total | 2 | 100.000 |
| Depth | Frequency | Percentage | |
|---|---|---|---|
| Bleeding | A | 2 | 100.000 |
| B | 0 | 0.000 | |
| Total | 2 | 100.000 | |
| Dry socket | A | 4 | 100.000 |
| B | 0 | 0.000 | |
| Total | 4 | 100.000 | |
| Muscle spasm | A | 4 | 66.667 |
| B | 2 | 33.333 | |
| Total | 6 | 100.000 | |
| Neurosensory change | A | 2 | 100.000 |
| B | 0 | 100.000 | |
| Total | 2 | 100.000 |
DISCUSSION
Our focus of this study was to determine the incidence of complications involved in the surgical removal of mandibular third molar in this center which included the intra-operative and post-operative complications.
Intra-operative complications
The intra-operative complications mostly included fracture of apical third of the root tip in three patients. All three subjects were informed and were consented for further follow-up. Retrieval of the root tip was successful in one subject without any damage to the supporting structures and secondary complications. With the rest of the two subjects, retrieval was not possible as they failed to report back to the department. Profuse bleeding occurred in 2 (0.8%) patients which is comparable to most of the studies. Both happened to be females who were above the age of 40 years, patients were reassured and bleeding was managed by applying pressure and using local hemostatic agents such as gel foam (Abgel).
Post-operative complications
On a general note, the post-operative complications had significant correlations with variables such as age, gender, spatial relationship, and the medical history of the patient. It was noted that the frequency of occurrence of complications increased with increase in age of the patient.[10] A statistically significant relation was also seen with gender. Majority of the cases with post-operative complications were males. Complications also seemed to be associated with pre-existing ailment in the patients such as type 2 diabetes. All the patients with post-operative complications had either a Distoangular or a Vertical type of impaction with Level A (high occlusal level) or Level B (medium occlusal level) and a difficulty score of either 5 or 6. So a significant relationship could be established between the post-operative complications and the difficulty level as all the cases were on the higher end of difficulty score.
Muscle spasm/trismus was the most common postoperative finding in our study. Trismus could have been caused due to hyperextension of temporalis muscle because of prolonged mouth opening, due to the inflammatory reaction after the surgery, hemorrhage, etc. The difficulty level could have been a factor for causing trismus. According to the literature, distoangular impaction has a significant association with post-operative trismus.[11,12] It can be prevented by practicing atraumatic injection and extraction techniques, avoiding multiple injections and avoiding very long surgical procedures. Patients with trismus were advised to practice mouth opening exercises, lateral excursions of mandible for 5 min every 2–3 h. Heat therapy and muscle relaxants were prescribed. Regular follow-up was done and it was noted that the condition of these subjects had improved after 2 weeks.
Dry socket was reported by four patients who were above the age of 40 years. These patients presented to the department with intense pain and the oral examination revealed the signs of dry socket. Out of 4 (1.6%) patients, three patients had given the history of diabetes type 2 and also had a history of smoking tobacco. Many studies have demonstrated a significant association between smoking and dry socket[4,13] and diabetes.[14] In our study, it was observed that there was a significant correlation between the systemic history, that is, type 2 diabetes as there is general compromise in the immunity that could have affected the healing process. Accordingly tobacco smoke contains chemical toxins that can delay healing. The use of prophylactic antibiotics for patients with diabetes before the surgery, avoiding smoking, following post-operative instructions, and maintaining good oral hygiene could prevent the occurrence of dry socket.[15] A thorough irrigation with betadine mouth wash was done for these patients, necessary antibiotics and analgesics were prescribed. Following this, the pain and infection was under control after 2 weeks of follow-up.
Temporary neurosensory changes were observed mostly in women (0.8%) who were above the age of 30 years. Temporary neurosensory change (paraesthesia or prolonged anesthesia) in the lingual nerve was seen in one patient. Patient reported with numbness in the tongue 2 days after the surgery. The most common causes include trauma to the nerve, injection of local anesthesia contaminated with alcohol, trauma to the nerve sheath, and hemorrhage around the nerve sheath[16]. Strictly following the injection procedure and proper handling of the cartridges will prevent the occurrence of such complications. The patient was reassured and was explained the causes of the problem. A nutritional supplement like neurobion forte was given for a month. After 2 months of follow-up, there were no signs of permanent damage to the nerve. The issue was resolved within 2 months.
The other subject presented with loss of muscle function of facial expressions; this was diagnosed as peripheral facial nerve paralysis. The palsy could be due to sympathetic vascular reflex, leading to ischemic paralysis in the stylomastoid foramen region. The anesthetic solution, its breakdown products, or even the mechanical action of the needle itself, may lead to stimulation of the sympathetic plexus. The stimulation of the plexus causes delayed reflex spasm of the vasa nervorum of the facial nerve, resulting in ischemic neuritis and secondary edema.[17] Transient facial nerve paralysis is almost always preventable by following the protocol of Inferior Alveolar Nerve block administration.[18] The patient was reassured and was explained that the problem was only temporary. However, the patient was monitored for few hours, after which it was noted that the patient had regained the normal muscle function.
The 2 (0.8%) patients who complained of post-operative bleeding were females above the age of 45 years; one of them with a history of hypertension and was on medication. Bleeding after dental extractions is sometimes affected by pharmacologic therapies like antiplatelet/anticoagulant/ anti-hypertensive drugs; literature reports show that dental extraction can be performed safely in patients treated with antiplatelet therapy.[19,20] Many other factors such as trauma to the extraction site, excessive spitting and use of straw could have also accounted for this complication.[21] Postoperative bleeding can be prevented by strictly following the post-operative instructions. The bleeding site was inspected, curated and finger pressure was applied to stop the blood from oozing out. Damp gauze was placed and the patient was monitored for 30 min after which it was noticed that bleeding had stopped.
Various literatures have reported complication rate around 37.4%[22] and 12%.[23] The overall rate of complications is less (7.6%) in our study. All the patients in our study were given prophylactic antibiotics and analgesics. The procedures were performed by skilled oral surgeons under aseptic conditions which could account for the lower rate of occurrence of complications. The major limitation of this study is that, the complication numbers obtained are very small, with this small number it is difficult to make correlations and come to any conclusions. The results obtained through this study can be befitting to this article but cannot be attributed to the population due to small complication numbers obtained.
CONCLUSION
There was a significant association to be found between the complication-rate and gender. Conditions such as muscle spasms/trismus and dry socket had a significant predilection towards the males while complications associated with neurosensory changes were commonly seen in females. There was also a significant association between habit history and rate of complication especially in conditions such as dry-socket where all the observed cases had positive history of tobacco/pan chewing habit. Interestingly, all the males who complained of dry socket also had reported medical history of type (2) diabetes. Patients with complications such as neurosensory changes were few and could have been prevented with good surgical skills and precision, moreover even if they were found they were temporary and treated with regular follow-up.
Acknowledgment
We would like to acknowledge the staff members of Oral and Maxillofacial Surgery Department for guiding us throughout the process. We also sincerely thank the interns and juniors posted in the department of Oral and Maxillofacial Surgery for assisting in collection and tabulation of data.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Incidence of impacted mandibular and maxillary third molars: A radiographic study in a Southeast Iran population. Med Oral Patol Oral Cir Bucal. 2013;18:e140-5.
- [CrossRef] [Google Scholar]
- The incidence of mandibular third molar impactions in different skeletal face types. Aust Dent J. 2008;53:320-4.
- [CrossRef] [Google Scholar]
- Complications of third molar extraction: A retrospective study from a tertiary healthcare centre in Oman. Sultan Qaboos Univ Med J. 2019;19:e230-5.
- [CrossRef] [Google Scholar]
- Complications after mandibular third molar extraction. Quintessence Int. 1995;26:779-84.
- [Google Scholar]
- Incidence of trismus in transalveolar extraction of lower third molar. J Pharm Bioallied Sci. 2017;9(Suppl 1):S222-7.
- [CrossRef] [Google Scholar]
- Does smoking increase the incidence of postoperative complications in simple exodontia? Int Dent J. 2012;62:106-8.
- [CrossRef] [Google Scholar]
- A retrospective study on the use of a dental dressing to reduce dry socket incidence in smokers. Gen Dent. 2015;63:17-21.
- [Google Scholar]
- Comparision of Healing of the Extraction Socket in Diabetic vs Non-Diabetic Patients.
- [Google Scholar]
- Transient delayed facial nerve palsy after inferior alveolar nerve block anesthesia. Anesth Prog. 2012;59:22-7.
- [CrossRef] [Google Scholar]
- Bleeding after tooth extraction in patients taking aspirin and clopidogrel (Plavix®) compared with healthy controls. Br J Oral Maxillofac Surg. 2016;54:568-72.
- [CrossRef] [Google Scholar]
- Complications associated with surgical removal of mandibular third molar: A prospective study. JNDA. 2020;19:10-5.
- [Google Scholar]
- The prophylactic extraction of third molars: A public health hazard. Am J Public Health. 2007;97:1554-9.
- [CrossRef] [Google Scholar]
- Iatrogenic root fracture secondary to extraction of impacted mandibular third molar that is masked by severe inflammation in the maxillofacial region a case report. Clin Case Rep Rev. 2018;4
- [CrossRef] [Google Scholar]
- Indications and risk factors for complications of lower third molar surgery in a Nigerian teaching hospital. Ann Med Health Sci Res. 2014;4:938-42.
- [CrossRef] [Google Scholar]
- Complications in surgical removal of mandibular third molars. Minerva Stomatol. 2009;58:359-66.
- [Google Scholar]
- Is short-term neurosensory testing after removal of mandibular third molars efficacious? Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 1998;85:366-70.
- [CrossRef] [Google Scholar]
- A clinical investigation into the incidence of dry socket. Br J Oral Maxillofac Surg. 1984;22:115-22.
- [CrossRef] [Google Scholar]
- Persistent trismus following mandibular third molar extraction and its management: A case report and literature review. World Acad Sci J. 2021;3:2.
- [CrossRef] [Google Scholar]
- Complications of impacted lower third molar surgery and its management a review. Eur J Mol Clin Med. 7:1597-602.
- [Google Scholar]
- Survey of Dental Services Rendered Unpublished Report. In: ADA Catalog No. SDSR. 1999.
- [Google Scholar]
- Pathological sequelae of “neglected” impacted third molars. Spiegel EH J Oral Pathol. 1988;17:113-7.
- [CrossRef] [Google Scholar]







