Translate this page into:
Aeronautics in dentistry: Navigating oral health challenges in zero gravity

*Corresponding author: Sandhya Tamgadge, Department of Oral and Maxillofacial Pathology, D.Y. Patil University School of Dentistry, Mumbai, Maharashtra, India. sandhya.tamgadge@dypatil.edu
-
Received: ,
Accepted: ,
How to cite this article: Doshi DJ, Tamgadge S. Aeronautics in dentistry: Navigating oral health challenges in zero gravity. J Academy Dent Educ. 2024;10:111-7. doi: 10.25259/JADE_36_2024
Abstract
Space, an expansive environment beyond Earth’s atmosphere, poses challenges for astronauts and spacecraft due to microgravity and radiation. These conditions disrupt saliva production, alter oral microbial composition, and challenge hygiene practices, leading to oral health concerns such as dental caries, periodontal diseases, and discomfort. Astronauts also face risks such as masticatory muscle atrophy and oral cancer during extended space missions. Thus, comprehensive dental care in space is crucial for astronaut well-being and overall health as humanity explores farther into space. This review delves into these challenges, exploring strategies to maintain optimal oral health during space travel and advancements in dental practices for astronauts on prolonged missions.
Keywords
Zero gravity
Aeronauts
Aeronautics in dentistry
Oral health
Aerospace
Oral hygiene
INTRODUCTION
Humans have always dreamed of the stars, and space exploration has advanced significantly since the late 20th century. The boundary of space is generally considered to be 100 km above sea level. Modern missions now allow for extended stays in space, bringing a range of environmental challenges such as microgravity, radiation, and temperature variations. These factors cause fluid shifts and musculoskeletal changes, profoundly affecting astronaut physiology and necessitating adaptation of vestibular and sensorimotor systems. Psychological impacts, changes in microbial flora, and compromised immunity are also critical considerations. Space exploration also impacts oral and maxillofacial health, leading to issues such as dental caries, periodontal diseases, jaw dysfunctions, and oral cancers. Addressing these orofacial issues is crucial for astronaut well-being. Aeronautical dentistry has emerged to focus on dental care in space, developing countermeasures for the physiological challenges faced during space travel. This field aims to ensure astronauts’ health and mission success.[1-6]
LITERATURE OF REVIEW
The field of aviation and space dentistry has evolved significantly since World War II. As aircraft began flying at higher altitudes, dental emergencies among flight crews increased, leading to the creation of dental research positions in aviation medicine. Over time, the focus expanded to include space pilots, with an emphasis on preventive care. Researchers developed guidelines for space dentistry and established training programs for astronauts. They also studied altitude-related dental pain, which was later termed “barodontalgia.”
As space missions became longer, maintaining oral health in zero-gravity environments became crucial. Researchers designed special dental instruments for use in space and investigated the effects of microgravity on the oral cavity. The term “aeronautic dentistry” was introduced, and educational programs in this field were established.
More recently, attention has turned to the impact of artificial intelligence on aviation, including how it might affect dental care in aerospace settings. Researchers are now examining whether university programs are adequately preparing graduates for these technological advancements in the aviation industry.[6,7]
DISCUSSION
The critical need for specialized space dentistry
National Aeronautics and Space Administration (NASA) enforces strict dental standards for astronauts, with examinations conducted 6 months before flight and treatments done 3 months prior, to minimize in-mission dental issues, and highlight the importance of space dentistry. However, microgravity poses significant oral health challenges, such as periodontitis, dental caries, bone loss, jaw fractures, pain, and numbness, especially during extended missions. With increasing space flights and future missions to the Moon, Mars, and beyond, dental emergencies will likely rise. Crews, despite operating in weightlessness, must be versatile and well-trained in handling medical and dental emergencies to ensure survival in space. Continued research in space dentistry is crucial for effective care and human survival during space exploration, offering valuable insights into human physiology and promoting advancements that benefit everyday life on Earth.[6,8]
Oral and maxillofacial transformations in spaceflight
Alveolar bone alterations in space
Human spaceflight leads to significant biological changes, such as bone loss and skeletal alterations due to microgravity.
Oral manifestations
Calcium depletion in astronauts leads to a condition known as osteoporosis. Microgravity impacts bone cell types, reducing osteoblast activity and responsiveness, leading to bone loss. Changes in bone density increase the risk of jaw and dental injuries.[5]
General manifestations
The reduced blood and plasma volume during space missions further alters bone deposition and resorption. NASA’s monitoring shows a 1–2% monthly bone mass loss in astronauts, with variations depending on location and stress levels.[9]
Studies at Johnson Space Center track changes in bone mineral density pre- and post-flight, revealing prolonged recovery periods. Research on cosmonauts shows that microgravity disrupts bone remodeling processes, contributing to bone loss and increased levels of certain enzymes and proteins in simulated microgravity conditions.[10]
Microbiome adaptations in space
Oral manifestations
Streptococcus dominated saliva (8% of species), with reduced diversity in space. Proteobacteria and Fusobacteria increased significantly in flight, while Actinobacteria decreased.
General manifestations
Taxa such as Catonella, Megasphaera, and Actinobacillus absent pre-flight appeared during flight, increasing in abundance for some participants.
Herpes virus reactivation in astronauts has been noted in various space missions and terrestrial experiments mimicking space conditions. Around 53% of astronauts in short-duration space shuttle flights showed herpes viruses in saliva or urine, with reactivations linked to mission duration. Reactivations of Epstein–Barr virus, cytomegalovirus (CMV), and varicella–zoster virus increased significantly in space, with CMV potentially contributing to immune dysfunction among crew members.[11,12]
Salivary adaptations in space
Studies on salivary changes in microgravity reveal altered bacterial profiles and increased risk of salivary stone formation due to calcium salt deposition. No significant pH or flow rate changes but noted shifts in oral bacteria. There are elevated levels of sodium, potassium, calcium, phosphate and proteins in saliva due to environmental and dietary factor due to microgravity. Saliva is increasingly studied in aerospace for its diagnostic potential, showing elevated antimicrobial proteins in ISS crew samples, highlighting its relevance in monitoring astronaut health during space missions.[13-15]
Immune system alterations due to radiation exposure in aerospace environments
Oral manifestations
While Earth-bound individuals typically encounter annual radiation exposures below 0.005 Sievert (Sv), International Space Station occupants face approximately 0.3 Sv annually.[4]
Space radiation, including ionizing particles from cosmic rays and solar flares, lacks Earth’s protective magnetosphere.[12] Studies indicate higher free radical activity in astronauts, with reduced levels of Vitamins E and C. Astronauts also face increased cancer risks from exposure to various toxins encountered in space missions, though current safety standards aim to limit this risk to 3% higher than that of the general population over their careers. Prolonged spaceflights may worsen these immune alterations, raising risks of malignancies.[16]
General manifestations
Space microgravity, along with stress, isolation, radiation, and disrupted rhythms, challenges the immune system. Studies show changes in white blood cell distribution, reduced T-cell effectiveness, and cytokine fluctuations during space flight, even in short missions.
Masticatory muscle atrophy and temporomandibular disorders (TMDs): Challenges in aerospace
In microgravity, antigravity muscles weaken due to reduced use, affecting limb muscles more than masticatory muscles like the masseter, which show stability. Philippou et al.’s research on mice aboard the Space Shuttle STS-135 revealed limb muscle mass loss and increased atrogene expression post-flight, contrasting with stable masseter muscles exhibiting enhanced signaling proteins. Microgravity reduces mechanical force, weakening bones and muscles, and increasing fracture risk. Disrupted circadian rhythms in space induce stress and sleep issues, impacting the temporomandibular joint and bone density. TMDs in space are linked to sleep disruptions and stress, affecting cortisol and melatonin levels and contributing to bruxism and dental problems.[5,17]
Decreased space pressure-decompression sickness (DCS)
Spaceflight can cause nitrogen to form microbubbles in tissues, leading to DCS due to decreased pressure. Gas emboli formation from rapid pressure drops compress nerves and blood vessels, following Boyle’s and Henry’s laws. DCS symptoms vary widely, affecting skin, joints, and major systems such as neurological and cardiac. Factors such as physical exertion and individual differences influence DCS risk in low-pressure environments. Astronauts use pure oxygen before extravehicular activities to release stored nitrogen and reduce DCS risk.[18]
Drug metabolism alterations
Oral manifestations
Medications may not work as effectively in space due to physiological changes and altered metabolism. Research by Idkaidek and Al-Ghazawi showed altered absorption rates of paracetamol during air travel, suggesting issues in space. These changes in drug absorption and metabolism can affect treatment efficacy and lead to drug accumulation.[19]
General manifestations
Crew members have reported dissatisfaction with some medications’ effectiveness during missions. A 1999 study by Putcha et al. documented cases where medications such as oxymetazoline, zolpidem, and aspirin were perceived as ineffective on Space Shuttle flights. Similarly, a 2014 study by Barger et al. noted that astronauts often needed a second dose of sleep-inducing drugs.[20-22]
Endodontic and periodontic issues in aerospace
Space conditions cause changes in bone density, salivary flow, immune functions, and oral microbiome, leading to endodontic and periodontic issues for astronauts. These problems worsen with subpar oral hygiene, stress, and fatigue. Pure oxygen exposure in space can corrode dental fillings. Psychological stress and disrupted sleep patterns contribute to bruxism, wearing down teeth and dental restorations.[14]
Baromatric pressure effects
Barotrauma, a condition arising from pressure differentials between the body’s gas-containing spaces and the surrounding atmosphere, is often encountered during high-altitude travel. This phenomenon is governed by Boyle’s law, which dictates that, under constant temperature conditions, the volume of gas is inversely proportional to the surrounding pressure.[14]
Dental barotrauma occurs when fluctuations in external barometric pressure cause damage to teeth or dental restorations. This can happen when a restored tooth contains a small void or gas pocket within the restoration, which expands or contracts in response to pressure changes, exerting enough force to potentially fracture the tooth or restoration. Reduced pressure in space can cause trapped gas to expand under dental restorations, leading to a condition known as odontocrexsis (tooth + explode). Calder and Ramsey emphasize the danger of subpar dental restorations, even without cavities, in causing dental injuries.[5]
Pain due to pressure changes in pulp
Barodontalgia is dental pain due to barometric pressure changes, often affecting a previously asymptomatic tooth. It is a symptom, not a separate condition, usually flaring up existing oral conditions such as caries, faulty restorations, pulpitis, necrosis, or periodontal issues. Barodontalgia comes in two types: “direct,” linked to tooth pulp or periapical issues, and “indirect,” caused by ear or sinus barotrauma. It can result from pressure changes due to decay or defects, leading to gas expansion under reduced pressure, discomfort, and organ dysfunction. As pressure drops during ascent, dissolved gasses in blood vessels may form bubbles in the pulp, worsening symptoms.[23,24]
Strategies and advancements
Dental emergencies in space missions can jeopardize success, making prevention and oral health crucial for astronauts. All crew members receive education on nutrition and oral hygiene, with regular checkups. NASA has strict criteria for astronaut selection and oral health monitoring, including annual clinical and radiographic examinations.[6]
Astronauts oral health classification
Astronaut class description
Class I: Good oral health; no need for dental treatment or reevaluation within 12 months
Class II: Some oral conditions present, but no imminent dental emergency expected within 12 months if left untreated
Class III: Oral conditions present, immediate dental treatment required to prevent a dental emergency within 12 months.[14]
All astronauts are required to maintain a minimum Class II dental status, with only those holding a Class I status before launch being considered for assignments on the International Space Station.
Six months before the scheduled launch, astronauts undergo a comprehensive dental examination. If any necessary dental interventions are identified, these procedures are scheduled and completed 3 months before launch to mitigate the risk of potential dental issues during the mission.[6]
During spaceflight, oral health checkups are done remotely using diagnostic systems, with oral cavity photos sent to ground control for assessment. The International Space Station has medical equipment and detailed instructions for dental emergencies such as crown replacement, tooth avulsion, and pain management. Dental protocols in space consider limitations such as water use and tool sharpening onboard spacecraft.[25]
Brushing teeth on space station
An astronaut [red arrow] floats weightlessly and with careful movements that they reach for a water bag [blue arrow]. Using a specialized nozzle, they release a controlled stream of water, forming delicate droplets. The astronaut deftly maneuvers the toothbrush toward the suspended droplets, allowing them to make contact with the bristles [yellow arrow]. Tiny spheres of water cling to the toothbrush, in the weightless environment. The toothpaste [NASA Dent] is typically contained in a sealed, squeezable tube with a nozzle that allows controlled dispensing. It utilizes a non-drip formula and a vacuum-sealed mechanism to prevent it from floating away or dispersing unintentionally and is always attached with a magnet to prevent it from floating elsewhere [green arrow].[26]
The toothpaste itself is formulated to be sticky and cohesive, ensuring it adheres to the bristles of the toothbrush when dispensed. Astronauts carefully squeeze a small amount onto their toothbrush, taking care to control the flow due to the absence of gravity. The sticky nature of the toothpaste helps it stay on the bristles, allowing astronauts to effectively clean[27] their teeth despite the challenges posed by microgravity[26] [Figure 1].
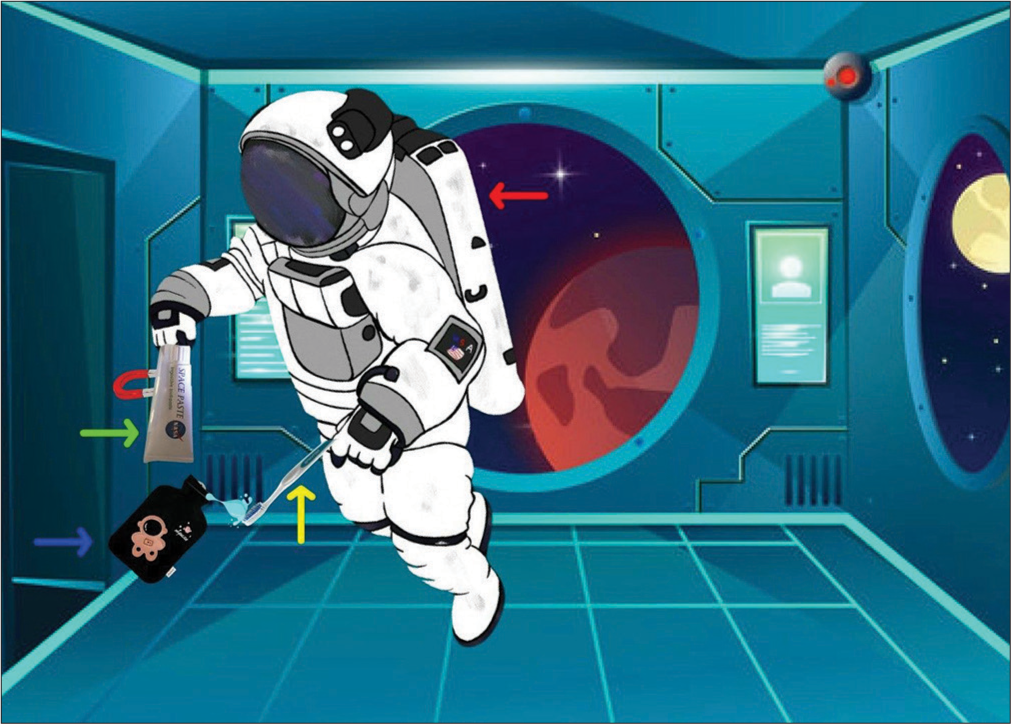
- Oral health procedures by astronauts in the confined quarters of the space shuttle. Red arrow- astronaut, blue arrow-waterbag, yellow arrow- bristles, green arrow-Nasadent toothpaste.
Pre-flight Precautions
Interventions for mitigating the risk of infection before space travel are described in this section:
The astronaut
Precautions for oral health
Temporary restorative materials are used on the International space station (ISS) but have durability constraints. Pre-flight endodontic treatments are recommended to prevent complications from pressure changes. Careful caries removal is crucial to avoid pulp exposure, necessitating complete root canal treatment before flight. Routine health screenings, including dental exams and tuberculosis tests, are essential. Resin cement is preferred for crown retention in space for its superior performance under pressure. Implant-supported prostheses are favored over removable dentures due to decreased barometric pressure affecting retention. Dentists must be cautious of oroantral communication risks during tooth extractions.[4]
Use of gloves during handling, safe waste disposal and optimal housing conditions are necessary to prevent disease transmission. Advanced bandages and sealants are used to minimize bleeding and maintain surgical sterility in microgravity, emphasizing safety for both patients and clinicians.[14,18]
General precautions
Astronauts require comprehensive vaccinations, including Measles, mumps, rubella (MMR), influenza, pneumococcal, meningococcal, hepatitis A and B, varicella zoster, and typhoid vaccines due to heightened risks on space missions.[28] Given the transmission of Staphylococcus aureus in space, astronauts should be screened for both methicillin-susceptible and methicillin-resistant strains using molecular methods. Screening for human immunodeficiency virus, latent fungal infections, and parasitic infections like Strongyloides is also recommended. Multiple stool samples should be checked for Salmonella. Infection control education and pre-launch isolation are crucial, and food irradiation, though impacting the gut microbiome, helps prevent contamination. All mission items must be sterilized for safety.[27,29-32]
The spacecraft or space habitat
Efforts to improve air quality and humidity in spacecraft include using high efficiency particulate air filters (HEPA) filters, despite energy challenges. Positive or neutral pressure after docking helps prevent airborne microbes, while separate pressure zones in bathrooms limit contaminant spread. Non-corrosive materials and antibiofouling coatings reduce biofilm in water systems, with water purification through pasteurization and submicron filters ensure safe drinking water. Foot-pedal-operated outlets minimize contamination risks. Coating spacecraft surfaces with nontoxic, antimicrobial materials prevents microbial growth. In addition, low-power portable ultraviolet light units can reduce surface microbial contamination, enhancing sanitation and safety for astronauts.[33-36]
Precautions during space travel
Precautions for oral health
Alcohol-based hand sanitizers are avoided in space; instead, benzalkonium chloride or chlorhexidine-based products are recommended. Spacecraft should be stocked with non-sterile and sterile gloves, antimicrobial agents, and cutaneous antiseptics. Maintaining oral hygiene with powered toothbrushes or chlorhexidine mouth rinses can reduce periodontal disease risk.[37-42]
General precautions
Astronauts with respiratory symptoms should wear surgical masks to prevent transmission, and proper cough etiquette is essential, especially when unmasked. Fit-tested N-95 respirators may be necessary for healthy astronauts if a colleague is symptomatic with an airborne pathogen. Germicidal wipes should clean high-touch surfaces and toileting devices after each use. Hand hygiene is crucial, with visual or audio reminders in bathrooms to prompt compliance. Regular environmental cleaning, air and water sampling, and exercise to boost immune function are essential. Probiotics like Lactobacillus may lower infection risk, and colonizing astronauts with beneficial Staphylococcus epidermidis could prevent harmful pathogen colonization. Astronauts receive extensive training in infection prevention and control for prolonged missions.[43-45]
Developing a specialized curriculum for aerospace dentistry
As spaceflight advances with upcoming missions to the Moon, Mars, and beyond, there is a critical need for a specialized postgraduate program in Aerospace Dentistry. This program would combine theoretical knowledge and practical training, preparing dentists to handle dental emergencies efficiently and to be well-prepared for space missions. The curriculum aims to equip dentists with the skills to address the unique challenges of space dentistry, ensuring they can respond to any situation. New oral hygiene devices tailored to microgravity environments, such as toothbrushes with suction capabilities and antimicrobial mouth rinses. Moreover, dietary modifications and personalized oral care regimens are being developed to mitigate the impact of space conditions on oral health. The mission is to train dentists in space-adapted practices, making them indispensable crew members, while the vision is to achieve academic excellence and enhance space crew well-being.
Future of aerospace dentistry
The future of aerospace dentistry hinges on technological advancements and understanding space’s impact on oral health. 3D printing will enable customized dental prostheses on-demand in space. Nanotechnology promises durable dental materials resilient to radiation. Tele-dentistry with AI and wearables will facilitate real-time dental consultations from Earth. Innovations such as personalized medicine and artificial gravity could transform aerospace dentistry. Addressing oral health challenges involves developing specialized oral hygiene devices and tailored care regimens for microgravity. Collaboration among dental experts, engineers, and space agencies is crucial for devising effective strategies to safeguard astronauts’ oral health during space missions.
CONCLUSION
This study illuminates the critical challenges and potential solutions for maintaining oral health in zero-gravity environments, crucial for long-duration space missions. Through comprehensive analysis of aeronautical principles applied to dentistry, novel strategies have been proposed to address issues such as microgravity-induced oral hygiene complications and dental emergencies. As humanity ventures further into space exploration, understanding and mitigating the unique oral health challenges in zero gravity will be imperative for ensuring the well-being and performance of astronauts. This interdisciplinary approach not only advances our knowledge of aeronautics in dentistry but also paves the way for innovative solutions benefiting both space exploration and terrestrial health-care practices.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Human health during space travel: State-of-the-art review. Cells. 2023;12:1-32.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term effects of microgravity and possible countermeasures. Adv Space Res. 1992;12:281-4.
- [CrossRef] [PubMed] [Google Scholar]
- The burden of space exploration on the mental health of astronauts: A narrative review. Clin Neuropsychiatry. 2021;18:237-46.
- [Google Scholar]
- Space and aeronautical dentistry: A review. Indian J Pharm Pharmacol. 2018;3:59-64.
- [CrossRef] [Google Scholar]
- Does microgravity effect on oral and maxillofacial region? Int J Astrobiol. 2020;19:406-12.
- [CrossRef] [Google Scholar]
- The history and importance of aeronautic dentistry. J Oral Sci. 2011;53:143-6.
- [CrossRef] [PubMed] [Google Scholar]
- Artificial intelligence in aviation: New professionals for new technologies. Appl Sci. 2023;13:11660.
- [CrossRef] [Google Scholar]
- Space exploration--surgical insights and future perspectives. Int J Surg. 2005;3:263-7.
- [CrossRef] [PubMed] [Google Scholar]
- Recovery of spaceflight-induced bone loss: Bone mineral density after long-duration missions as fitted with an exponential function. Bone. 2007;41:973-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bone formation and resorption biological markers in cosmonauts during and after a 180-day space flight (Euromir 95) Clin Chem. 1998;44:578-85.
- [CrossRef] [PubMed] [Google Scholar]
- The influence of spaceflight on the astronaut salivary microbiome and the search for a microbiome biomarker for viral reactivation. Microbiome. 2020;8:56.
- [CrossRef] [PubMed] [Google Scholar]
- Herpes virus reactivation in astronauts during spaceflight and its application on earth. Front Microbiol. 2019;10:16.
- [CrossRef] [PubMed] [Google Scholar]
- Short-term head-down bed rest microgravity simulation alters salivary microbiome in young healthy men. Front Microbiol. 2022;13:1056637.
- [CrossRef] [PubMed] [Google Scholar]
- Salivary antimicrobial proteins and stress biomarkers are elevated during a 6-month mission to the international space station. J Appl Physiol (1985). 2019;128:264-75.
- [CrossRef] [PubMed] [Google Scholar]
- Masticatory muscles of mouse do not undergo atrophy in space. FASEB J. 2015;29:2769-79.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of flying at high altitude on early exposure of paracetamol in humans. Drug Res (Stuttg). 2019;69:348-51.
- [CrossRef] [PubMed] [Google Scholar]
- Pharmaceutical use by U.S. astronauts on space shuttle missions. Aviat Space Environ Med. 1999;70:705-8.
- [Google Scholar]
- Prevalence of sleep deficiency and use of hypnotic drugs in astronauts before, during, and after spaceflight: An observational study. Lancet Neurol. 2014;13:904-12.
- [CrossRef] [PubMed] [Google Scholar]
- Physiological adaptations affecting drug pharmacokinetics in space: What do we really know? A critical review of the literature. Br J Pharmacol. 2022;179:2538-57.
- [CrossRef] [PubMed] [Google Scholar]
- Aviation dentistry: Current concepts and practice. Br Dent J. 2009;206:11-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dental treatment during a human mars mission with remote support and advanced technology In: 46th international conference on environmental systems. 2016. p. :1-11. Available from: https://hdl.handle.net/2346/67570 [Last accessed on 2024 Jun 20]
- [Google Scholar]
- Is oral health affected in long period space missions only by microgravity? A systematic review. Acta Astronaut. 2020;167:343-50.
- [CrossRef] [Google Scholar]
- Carriage rates of methicillin-resistant Staphylococcus aureus (MRSA) depend on anatomic location, the number of sites cultured, culture methods, and the distribution of clonotypes. Eur J Clin Microbiol Infect Dis. 2010;29:1553-9.
- [CrossRef] [PubMed] [Google Scholar]
- Asymptomatic reactivation and shed of infectious varicella zoster virus in astronauts. J Med Virol. 2008;80:1116-22.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of Staphylococcus aureus during space flight. FEMS Immunol Med Microbiol. 1996;16:273-81.
- [CrossRef] [PubMed] [Google Scholar]
- Serum KL-6 level as a monitoring marker in a patient with pulmonary alveolar proteinosis. Thorax. 1998;53:809-11.
- [CrossRef] [PubMed] [Google Scholar]
- Efficiency of cultures of rectal swabs and faecal specimens in detecting Salmonella carriers: Correlation with numbers of Salmonellas excreted. J Hyg (Lond). 1966;64:261-9.
- [CrossRef] [PubMed] [Google Scholar]
- The World Health Organization guidelines on hand hygiene in health care and their consensus recommendations. Infect Control Hosp Epidemiol. 2009;30:611-22.
- [CrossRef] [PubMed] [Google Scholar]
- Outbreak of Shigella sonnei in a clinical microbiology laboratory. J Clin Microbiol. 1997;35:3163-5.
- [CrossRef] [PubMed] [Google Scholar]
- Design of antibacterial surfaces and interfaces: Polyelectrolyte multilayers as a multifunctional platform. Macromolecules. 2009;42:8573-86.
- [CrossRef] [Google Scholar]
- Analysis of a spacecraft life support system for a Mars mission. Acta Astronaut. 2004;55:537-47.
- [CrossRef] [PubMed] [Google Scholar]
- Room decontamination with UV radiation. Infect Control Hosp Epidemiol. 2010;31:1025-9.
- [CrossRef] [PubMed] [Google Scholar]
- High-dose vitamin D(3) during intensive-phase antimicrobial treatment of pulmonary tuberculosis: A double-blind randomised controlled trial. Lancet. 2011;377:242-50.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the use of different modes of mechanical oral hygiene in prevention of plaque and gingivitis. J Periodontol. 2008;79:1386-94.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical efficacy of antimicrobial mouthrinses. J Dent. 2010;38(Suppl 1):S6-10.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of visual cues to improve hand hygiene compliance. Simul Healthc. 2010;5:325-31.
- [CrossRef] [PubMed] [Google Scholar]
- Microbiological status of cosmonauts during orbital spaceflights on Salyut and Mir orbital stations. Acta Astronaut. 2005;56:839-50.
- [CrossRef] [PubMed] [Google Scholar]
- Staphylococcus epidermidis Esp inhibits Staphylococcus aureus biofilm formation and nasal colonization. Nature. 2010;465:346-9.
- [CrossRef] [PubMed] [Google Scholar]
- A quantitative assessment of the efficacy of surgical and N95 masks to filter influenza virus in patients with acute influenza infection. Clin Infect Dis. 2009;49:275-7.
- [CrossRef] [PubMed] [Google Scholar]
- Measurements of airborne influenza virus in aerosol particles from human coughs. PLoS One. 2010;5:e15100.
- [CrossRef] [PubMed] [Google Scholar]
- Preventing the spread of influenza A H1N1 2009 to health-care workers. Lancet Infect Dis. 2009;9:723-4.
- [CrossRef] [PubMed] [Google Scholar]







