Translate this page into:
To evaluate and compare the effect of diabetes and complete denture wearing on the occurrence of Mucor isolates in edentulous geriatric patients

*Corresponding author: Bhupender Yadav, Professor and Head, Department of Prosthodontics, Shree Guru Gobind Singh Tricentenary University, Gurgaon, Haryana, India. drbhupinderyadav@gmail..com
-
Received: ,
Accepted: ,
How to cite this article: Yadav K, Yadav B, Malhotra T, Sardar M, Nagpal A, Shetty O. To evaluate and compare the effect of diabetes and complete denture wearing on the occurrence of Mucor isolates in edentulous geriatric patients. J Academy Dent Educ. 2024;10:93-9. doi: 10.25259/JADE_91_2023
Abstract
Objectives:
The objective of this study was to explore the impact of diabetes and complete denture use on the presence of Mucor isolates in edentulous geriatric patients.
Material and Methods:
Intraoral swab samples were collected using a sterile culture device, focusing on the center of the hard palate for all patient groups. Immediately after collection, each sample was immersed in a sterile culture-collecting device containing normal saline to prevent swab drying. Subsequently, these swabs were isolated and cultured in Sabouraud’s dextrose agar medium at a temperature range of 25–30°C.
Results:
Statistical analysis using the Chi-square test revealed no Mucor isolates in any of the four groups. However, the combination of diabetes and complete denture use led to the isolation of other commensal fungi in 65% of samples, contrasting with the non-diabetic, non-denture-wearing group where this occurrence was only 5%.
Conclusion:
The study concluded that there was no observable correlation between the occurrence of Mucor isolates in edentulous geriatric patients, irrespective of complete denture use, or diabetic status. Nevertheless, the coexistence of diabetes and complete denture use significantly increased the presence of opportunistic fungi in the oral cavity compared to non-diabetic, non-denture-wearing patients.
Keywords
Edentulous
Geriatric
Denture
Isolation
Diabetes
INTRODUCTION
Diabetes, a prevalent chronic metabolic ailment impacting individuals across all age groups, leads to elevated blood glucose levels and consequential damage to vital organs, including the heart, blood vessels, eyes, kidneys, and nerves, as defined by the World Health Organization.[1] In the post-COVID era, immunity has markedly decreased, rendering individuals with diabetes more susceptible to opportunistic infections such as mucormycosis and candidiasis. The compromised immune function in diabetes exacerbates the risk of infections. Vigilant management of diabetes, including the maintenance of optimal blood glucose levels and the adoption of a healthy lifestyle, is crucial. Moreover, health-care providers must be attentive to diabetes-related complications and the heightened susceptibility to infections. Proactive measures, such as vaccination and adherence to hygiene practices, are essential in reducing the risk of opportunistic infections in individuals with diabetes. Comprehensive public health initiatives and educational campaigns are pivotal for enhancing awareness and understanding of diabetes and its complications, especially in the context of the enduring global health challenges post-COVID-19.
The global upheaval caused by the COVID tsunami prompted the widespread use of excessive steroids, resulting in a population with compromised immunity. This susceptibility gave rise to opportunistic infections, with Mucormycosis spreading rapidly and impacting both the country’s economy and the health-care sector.[2] The surge in Mucormycosis cases appears to be multifactorial, influenced by factors such as innate and acquired immunosuppression. Although diabetes mellitus (DM) stands out as the most common underlying medical comorbidity in affected patients, the intricate oral microbial ecology plays a role.[3]
The oral cavity consists of complex oral microflora, comprising various bacterial species, mycoplasma, fungi, and protozoa. Candida albicans, Aspergillus, Mucor, and other fungi are commonly present as opportunistic pathogens in the oral cavities of healthy individuals. These pathogens can cause diverse fungal infections in people with weakened immune systems due to various reasons. Research by Pallavan et al.[4] revealed that healthy individuals exhibit lower colonization of candida in the oral cavity compared to those with diabetes. Balan et al.[5] noted that the oral environment undergoes changes and becomes more acidic in individuals with diabetes during hyperglycemic episodes. This alteration facilitates the transition of commensal fungi to pathogens, with fungi exhibiting a heightened ability to adhere to the epithelium and denture surfaces at low pH levels ranging from 2 to 4.
Numerous studies[6,7] highlight that the microbial flora undergoes both qualitative and quantitative changes in response to various factors such as food consumption, eruption of tooth, tooth exfoliation, the use of dentures, and the frequency of denture use. Fungi’s attachment to the intaglio surface of the dentures acts as an efficient niche for microorganisms, contributing to fungal infections in individuals who wear dentures. The interplay of attractive hydrophobic and repellent electrostatic forces has been associated with the ability of fungi to adhere to polymeric surfaces. The surface properties of acrylic materials play a crucial role in the adhesion of fungi to denture base resin, creating opportunities for further bonding and colonization.[8]
The connection between DM and fungal infections, such as candidiasis, is well-established. However, there is limited scientific literature on the correlation between diabetes and mucormycosis. Furthermore, the relationship between complete denture wearing and an individual’s diabetic status concerning the occurrence of opportunistic fungi, like Mucor, in the oral cavity is not well-explored. Therefore, the objective of this study was to assess the impact of denture wearing and diabetes on the presence of Mucor isolates in the oral cavity. The null hypothesis posited that there would be no significant difference in the occurrence of Mucor isolates, regardless of an individual’s diabetic and complete denture-wearing status.
MATERIAL AND METHODS
A total of 80 edentulous patients were selected and divided into four groups of 20 patients each based on inclusion and exclusion criteria. The patients were recruited from the outpatient department of Prosthodontics, Faculty of Dental Science to participate in the study for 2–3 months according to the following inclusion and exclusion criteria:
Inclusion criteria
The following criteria were included in the study:
Age range of 60–80 years
Edentulous patients
No other comorbidity
Patients should have good oral hygiene and clinically normal oral mucosa
Patient should be non-allergic (had no past history of allergy to drugs, materials, foodstuff)
Patient should not have any oral lesions when examined intraorally.
Exclusion criteria
The following criteria were excluded from the study:
Patients with advanced degrees of pulmonary, renal, endocrine, or cardiac insufficiency
Dentulous patients
Allergy to materials used in the study
Current drug abuse
Severe salivary gland dysfunction.
The study was approved by the Institutional Ethical Committee for the use of human subjects with an ethical clearance number FODS/EC/ICMR-STS/2022/04.
Two clinical tests were used to assess the diabetic status of the individual, that is, fasting serum glucose concentration and glycosylated hemoglobin concentration through blood investigations. The patients were explained the complete procedure and treatment planning and, further, procedures were performed after the patient’s consent.
Sample size calculation
The sample size was calculated using the following formula, that is,
Considering α error only,
α = 5%
Z = 1.96 (Constant value)
P = expected proportion/prevalence = 12%
d = precision, that is, 7%
level of confidence = 95%
= 82 which was rounded off to 80.
The patients were divided into four groups of 20 each:
Group 1 (n = 20): Non-diabetic edentulous patient not wearing complete dentures
Group 2 (n = 20): Non-diabetic edentulous patient wearing complete dentures
Group 3 (n = 20): Diabetic edentulous patients not wearing complete dentures
Group 4 (n = 20): Diabetic edentulous patients wearing complete dentures
Collection of swab samples
The mycological testing material was obtained using a standardized protocol. Before examination, patients were instructed to refrain from engaging in hygienic practices, eating, drinking, and smoking and were required to remove their dentures before the morning examination. Swab samples were intraorally collected using a sterile culture device [Figure 1]. Uniformly, swabs were obtained from the central area of the hard palate across all patient groups [Figure 2]. Immediately on collection, each sample was immersed in a sterile culture-collecting device containing normal saline to prevent desiccation. The samples were promptly dispatched to the department of microbiology, where they were transferred to Sabouraud’s medium and incubated at 25°C. Inspection of the samples occurred after 24 and 48 h.[9]
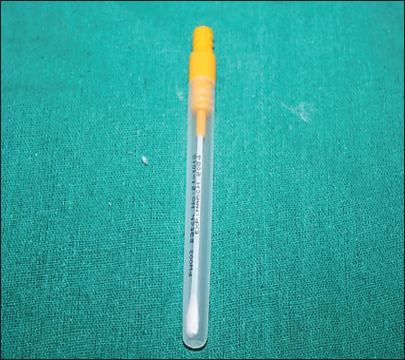
- Armamentarium used for collection of swab sample.
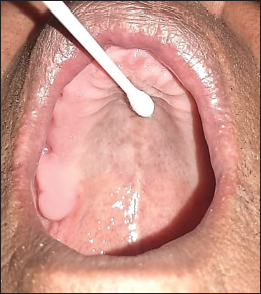
- Collection of swab sample from hard palate.
Preparation of Sabouraud dextrose agar (SDA)
The SDA media was prepared by combining all the ingredients, including Peptone (derived from Enzymatic Digest of Casein and Enzymatic Digest of Animal Tissue), Dextrose (added as the energy and carbon source), and Agar (used as the solidifying agent), in approximately 900 mL of deionized water. The pH of the mixture was adjusted to 5.6 using hydrochloric acid, and the final volume was set at 1 L. The mixture was then heated to facilitate the complete dissolution of the medium. Following this, it underwent autoclaving at 121°C for 15 min and was subsequently cooled to around 45–50°C. This process ensured the preparation of a sterile and suitable medium for mycological testing.[10,11]
Result interpretation on SDA
Following the appropriate incubation period, the observed growth or colonies underwent analysis through Gram staining and were examined under a microscope (Nikon, Eclipse E100) for microscopic assessment. In addition, a comprehensive biometric analysis was conducted to confirm fungal growth and identify the specific species. The identification process involved observing various colony characteristics, morphological features, distinctive microscopic structures, growth rates, preferred media for organism growth, and the specimen’s source.[12] The results were typically obtained within a span of 3–5 days [Figure 3].
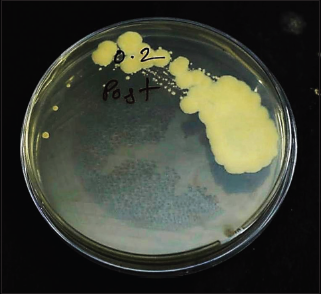
- Growth of fungal isolate (other than Mucor) in diabetic denture wearing individual.
Subsequently, on obtaining the results, a statistical analysis was carried out, and a comparative evaluation was performed using the Chi-square test to assess any significant differences or associations. This systematic approach ensured a thorough examination and interpretation of the mycological findings.
RESULTS
The Chi-square test was used to calculate P-value by comparing the value of the statistic to a Chi-square distribution. The number of degrees of freedom is equal to the number of possible outcomes, minus 1. The results revealed that there were no significant values of Mucor isolates that were found in any of the four groups. Whereas, other fungal isolates were observed mainly among the diabetic and denture-wearer groups and less significantly among the non-diabetic and non-denture wearer groups.
DISCUSSION
The majority of fungi are potential pathogens and commonly coexist within the human body’s flora.[13] Opportunistic fungal infections earn their designation because these fungi exploit the host’s vulnerability as an advantageous circumstance. Both fungi, particularly yeasts, and bacteria significantly contribute to the initiation, exacerbation, and perpetuation of denture stomatitis.[14,15]
Immunosuppression, extensive use of steroids in COVID-19 treatment, poorly controlled DM, hematological malignancy, solid organ transplant, and DM are identified as the primary risk factors for opportunistic fungal infections. Following closely are hypertension and other comorbidities in second and third place.[16] Studies have also demonstrated that conditions such as acidosis and hyperglycemia hinder the ability of phagocytes to eliminate fungal spores through oxidative and non-oxidative processes.[17]
Elevated blood glucose levels, known as hyperglycemia, are a recognized side effect of systemic steroid use. A recent study indicated that 84.3% of patients included in the research had used steroids, with methylprednisolone being the most commonly employed steroid (66.8%). The majority of patients had been on a steroid regimen for a duration of 7–14 days. Among the participants, 204 individuals were identified with diabetes, and notably, 42.1% of them had received a recent diagnosis either before or after undergoing COVID-19 treatment.
Interestingly, the present study did not find a correlation between the occurrence of Mucor isolates in edentulous geriatric patients, both with and without diabetes. The null hypothesis was accepted [Table 1]. One potential explanation for this outcome could be the absence of steroid usage in the studied population. Consequently, the immune systems of these individuals may not have been significantly compromised, thereby reducing the likelihood of Mucor isolates being present in the swabs collected from the patients’ hard palates.
| Group | Mucor isolates (Absent) (%) | Mucor isolates (Present) (%) | Chi-square | P-value |
|---|---|---|---|---|
| Group 1 (Nondiabetic and Nondenture wearer) | 20 (100) | 0 (0) | Here variable is constant. Chisquare Test cannot be performed |
------------------ |
| Group 2 (Nondiabetic and Denture wearer) | 20 (100) | 0 (0) | ||
| Group 3 (Diabetic and Nondenture wearer) | 20 (100) | 0 (0) | ||
| Group 4 (Diabetic and Denture wearer) | 20 (100) | 0 (0) |
In addition, various fungal isolates such as C. albicans, Aspergillus, Aureobasidium, and Cryptococcus are prevalent as opportunistic fungal pathogens in the oral cavity, leading to a spectrum of fungal infections. C. albicans continues to be the most frequently isolated fungus in the oral cavity, although other species have also been identified, with associations to various ailments. Denture wearers, in particular, exhibit a higher frequency of fungal isolates due to increased adherence of fungi to the rough tissue surface of the denture base, forming an efficient reservoir for microorganisms [Table 2].[18]
| Group | Other fungal isolates (Absent) (%) | Other fungal isolates (Absent) (%) | Chi-square | P-value |
|---|---|---|---|---|
| Group 1 (NonDiabetic and NonDenture Wearer) | 19 (95) | 01 (5) | 9.800 | 0.002* |
| Group 2 (NonDiabetic and Denture Wearer) | 18 (90) | 02 (10) | ||
| Group 3 (Diabetic and NonDenture Wearer) | 10 (50) | 10 (50) | ||
| Group 4 (Diabetic and Denture Wearer) | 07 (35) | 13 (65) |
The findings of the current research support this observation and validate the presence of various commensal fungi, including Mucor, in the collected samples. Fungal isolates were notably more prevalent among denture wearer groups [Figure 3]. Approximately 5% of participants in the non-diabetic and non-denture wearer groups showed the presence of fungal isolates [Table 3], while the percentage increased to 10% in the non-diabetic and denture wearing group [Table 4]. Notably, among diabetic individuals who did not wear dentures, fungal isolates were present in 50% of the cases [Table 5], and in diabetic individuals who were denture wearers, the incidence rose to 65% [Table 6]. These differences were statistically significant when comparing the various groups.
| Frequency | Percentage | Chi-square | P-value | |
|---|---|---|---|---|
| Mucor isolate | ||||
| No | 20 | 100 | Here variable is constant. Chi-square test cannot be performed |
|
| Yes | 00 | 00 | ||
| Other Isolate | ||||
| No | 19 | 95.0 | 16.20 | 0.000* |
| Yes | 1 | 5.0 | ||
| Frequency | Percentage | Chi-square | P-value | |
|---|---|---|---|---|
| Mucor isolate | ||||
| No | 20 | 100 | Here variable is constant. Chi-square test cannot be performed |
|
| Yes | 00 | 00 | ||
| Other | ||||
| No | 18 | 90.0 | 12.280 | 0.000 |
| Yes | 2 | 10.0 | ||
| Frequency | Percentage | Chi-square | P-value | |
|---|---|---|---|---|
| Mucor isolate | ||||
| No | 20 | 100 | Here variable is constant. Chi-square test cannot be performed |
|
| Yes | 00 | 00 | ||
| Other | ||||
| No | 10 | 50.0 | 0.00 | 1.00 |
| Yes | 10 | 50.0 | ||
| Frequency | Percentage | Chi-square | P-value | |
|---|---|---|---|---|
| Mucor isolate | ||||
| No | 20 | 100 | Here variable is constant. Chi-square test cannot be performed |
|
| Yes | 00 | 00 | ||
| Other | ||||
| No | 7 | 35.0 | 16.200 | 0.00* |
| Yes | 13 | 65.0 | ||
Over the past 2 years, particularly in the post-COVID period, there has been a notable increase in the frequency of both superficial and invasive opportunistic fungal infections. Opportunistic fungal diseases are demonstrating a shift in their prevalence.[19] While Candida species continue to be the primary culprits behind invasive fungal infections, infections caused by other mycelial fungi such as Aspergillus and Mucor are on the rise. This study has provided evidence supporting the notion that denture wearing in conjunction with diabetes can be a significant factor in the presence of various fungal species in the oral cavity. Such presence could potentially lead to life-threatening diseases if the patient’s immune system becomes compromised for any reason.
It is imperative for individuals with diabetes wearing complete dentures to be informed about proper denture hygiene practices. Specifically, avoiding wearing dentures at night and utilizing commercially available denture cleansers for effective cleaning can help prevent the adherence of microorganisms on the denture surface.[20,21] These instructions should be reiterated during each follow-up visit, and if any signs or symptoms of infection arise, prompt treatment is crucial.
It is worth noting that the study may have limitations, such as a relatively small sample size and the exclusion of other factors that could contribute to variations in fungal growth, such as the patient’s oral hygiene and medication. Future studies or clinical trials with larger and more diverse populations, including individuals with uncontrolled diabetes, those with diabetes taking steroids, or immunocompromised patients, should be conducted to draw more specific conclusions.
CONCLUSION
The present study concluded that there was no correlation between the occurrence of Mucor isolates in edentulous geriatric patients with or without wearing complete dentures and irrespective of diabetic status. However, diabetes and complete denture-wearing results in a significantly increased presence of other opportunistic fungi in the oral cavity when compared to non-diabetic and non-denture-wearing patients.
Acknowledgement
This research was funded by ICMR under STS scheme provided to undergraduate students and authors are thankful for the financial support provided and for promotion of research at undergraduate level.
Ethical approval
The research/study approved by the Institutional Review Board at SGT University, number FODS/EC/ICMRSTS/2022/04, dated 05/06 April 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Financial support from ICMR under STS Scholarship.
References
- Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215-22.
- [CrossRef] [PubMed] [Google Scholar]
- Zygomycosis in Europe: Analysis of 230 cases accrued by the registry of the European confederation of medical mycology (ECMM) working group on zygomycosis between 2005 and 2007. Clin Microbiol Infect. 2011;17:1859-67.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical study to assess the breath protection efficacy of denture adhesive. J Contemp Dent Pract. 2002;3:1-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison and correlation of candidal colonization in diabetic patients and normal individuals. J Diabetes Metab Disord. 2014;13:66.
- [CrossRef] [PubMed] [Google Scholar]
- Candida carriage rate and growth characteristics of saliva in diabetes mellitus patients: A case-control study. J Dent Res Dent Clin Dent Prospect. 2015;9:274-9.
- [CrossRef] [PubMed] [Google Scholar]
- Mucormycosis: Oral and prosthodontic implications. A report of 14 patients. J Prosthet Dent. 1982;47:422-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes and mucormycosis: A complex interplay. Diabetes Metab. 2012;38:193-204.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of denture wearing on occurrence of fungal Isolates in the oral cavity: A pilot study. J Clin Exp Dent. 2012;4:e86-90.
- [CrossRef] [PubMed] [Google Scholar]
- Mucormycosis in a diabetic ketoacidosis patient. Asian Pac J Trop Biomed. 2013;3:830-3.
- [CrossRef] [PubMed] [Google Scholar]
- Mucormycosis in a diabetic patient: A case report with an insight into its pathophysiology. Contemp Clin Dent. 2017;8:662-6.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of prosthodontic treatment on the oral health-related quality of life in mucormycosis patient: A case report. Cureus. 2018;10:3493-9.
- [CrossRef] [PubMed] [Google Scholar]
- Diabetes mellitus as the major risk factor for mucormycosis in Mexico: Epidemiology, diagnosis, and outcomes of reported cases. Med Mycol. 2018;56:29-43.
- [CrossRef] [PubMed] [Google Scholar]
- The association of denture stomatitis and partial removable dental prostheses: A systematic review. Int J Prosthodont. 2012;25:113-9.
- [Google Scholar]
- Hygiene practices in removable prosthodontics: A systematic review. Int J Dent Hyg. 2018;16:179-201.
- [CrossRef] [PubMed] [Google Scholar]
- A comparative study for plaque removing efficacy between commonly used denture cleansers in India. J Indian Prosthodont Soc. 2017;17:295-300.
- [CrossRef] [PubMed] [Google Scholar]
- Quality management in healthcare: The pivotal desideratum. J Oral Biol Craniofac Res. 2019;9:180-2.
- [CrossRef] [PubMed] [Google Scholar]
- Rhino-orbital-cerebral-mucormycosis in COVID-19: A systematic review. Indian J Pharmacol. 2021;53:317-27.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19, diabetes and steroids: The demonic trident for mucormycosis. Indian J Otolaryngol Head Neck Surg. 2022;74:3469-72.
- [CrossRef] [PubMed] [Google Scholar]
- Uncommon opportunistic fungal infections of oral cavity: A review. J Oral Maxillofac Pathol. 2014;18:235-43.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid hyperglycemia: Prevalence, early detection and therapeutic recommendations: A narrative review. World J Diabetes. 2015;6:1073-81.
- [CrossRef] [PubMed] [Google Scholar]
- Steroid-induced diabetes: A clinical and molecular approach to understanding and treatment. Diabetes Metab Res Rev. 2014;30:96-102.
- [CrossRef] [PubMed] [Google Scholar]







