Translate this page into:
Temporomandibular joint reankylosis: A case report
*Corresponding author: Kruthika Murali, Associate professor, Department of Pedodontics and Preventive Dentistry, Vinayaka Mission’s Sankarachariyar Dental College, Vinayaka Mission’s Research Foundation (Deemed to be University), Salem, Tamil Nadu, India. smilekruthika@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Valluvan S, Murali K, Duraisamy V, Gopalam T. Temporomandibular joint reankylosis: A case report. J Academy Dent Educ 2020;6(1 & 2):35-40.
Abstract
Ankylosis of the temporomandibular joint (TMJ) occurs when the base of the skull fuses with condyle to the mandible. This can cause deleterious effects on the growth and development of the jaws and teeth when occurred in childhood. Recurrence of TMJ ankylosis is a known complication. Studies have contributed to the various treatment options in recurrent ankylosis. The causes of reankylosis of TMJ are due to inadequate gap arthroplasty, insufficient interpositional material, adhesion, and elongation of the coronoid process. This case report is about a 6-year-old female child who is not able to open the mouth. The child was diagnosed with TMJ reankylosis. The treatment consisted of gap arthroplasty with dermis-fat graft along with bilateral coronoidectomy followed by vigorous physiotherapy. Later, full-mouth rehabilitation with speech and functional therapy and psychological counseling was done. Treating TMJ ankylosis is challenging as it has technical difficulties and a high incidence of recurrence. Hence, the treatment is always a multidisciplinary approach inclusive of an oral and maxillofacial surgeon, a pediatric dentist, and a psychologist and a physical therapist.
Keywords
Ankylosis
Reankylosis
Case report
Gap arthroplasty
Temporomandibular joint
INTRODUCTION
Ankylosis is a Greek word meaning “stiff joint.” Temporomandibular joint (TMJ) ankylosis is defined as bony or fibrous adhesion of the components of TMJ associated with limitation in opening the mouth, causing difficulties with mastication, speaking, and oral hygiene and also inadvertently influences the mandibular growth.[1] TMJ ankylosis occurs due to trauma, systemic diseases, or local or systemic infection. Ankylosis can also occur as a result of TMJ surgery.[2-5] The male:female ratio is 1:9 in children with most patient’s (70%) being in 10–15 years age group (mean age 11.1 years ± 3.34 years).[6] In India, the prevalence of TMJ ankylosis tends to be high among growing children.
The etiology includes congenital-abnormal uterine development and birth injuries and acquired trauma, malunion of condylar fractures, and inflammation of joint.[7]
Pathologically, atrophic changes are seen in the cartilaginous components of the joint with loss of meniscus. Progressive destruction of joint tissues with narrowing of joint space occurs. Normal soft tissues are replaced by thick fibrous bands. Bony changes are characterized by overall flattening of articulation. Glenoid fossa and articular eminence become less pronounced. Condyle becomes enlarged, composing of dense sclerotic bone. Ultimately bony fusion takes place between articular surfaces. The normal anatomical features are obscured by dense bone and joint space gets obliterated.[1]
Management involves an interdisciplinary approach. Various authors prefer different modes of treatment based on the severity of TMJ ankylosis. Some of them are
Coronoidectomy +Condylectomy +Physiotherapy(or)
Condylectomy +Gap arthroplasty +Physiotherapy(or)
Condylectomy +Joint reconstruction with costochondral graft +Physiotherapy.[8]
CASE REPORT
A 6-year-old female child came to the Department of Pedodontics and Preventive Dentistry, Vinayaka Mission’s Sankarachariyar Dental College, Salem, with the chief complaint of difficulty in opening the mouth. The patient was apparently normal 1 year back then she noticed difficulty in opening the mouth so the child was not able to masticate food, limiting her intake to liquid or semisolids.
The patient had no significant past trauma or medical history. Her dental history revealed that she underwent a surgery 1 year back for ankylosis but it was not stable and she presented with condition termed reankylosis.
There was no family history of congenital disorders. The child had natural delivery and her parents were nonconsanguineous.
The initial examination revealed a retrognathic mandible with Class II relationship [Figures 1-3]. On extraoral examination, the face appeared asymmetrical with fullness of cheek and deviation of mandible and chin to the right with lower facial asymmetry [Figure 1] with mouth opening restricted to 0.5 mm [Figure 4]. Radiographic investigations included orthopantomogram and computed tomography (CT) [Figure 5-7].

- Facial view.

- Right lateral view side.

- Left lateral view.
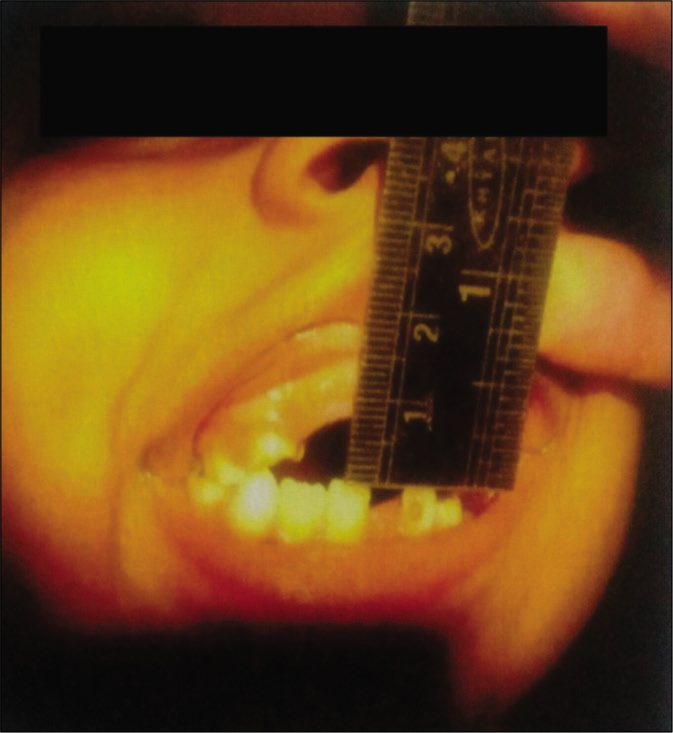
- Mouth opening: 0.5 mm.
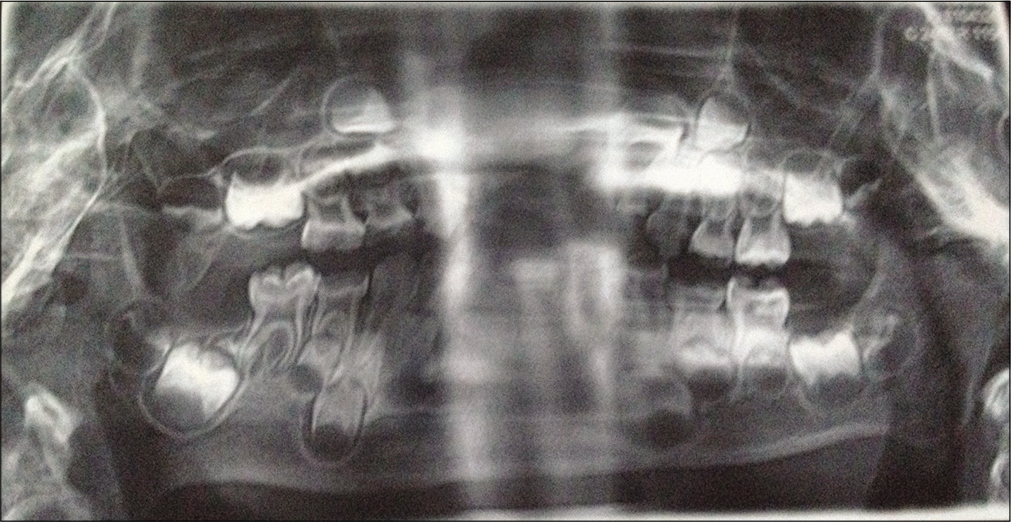
- Pre-operative OPG.
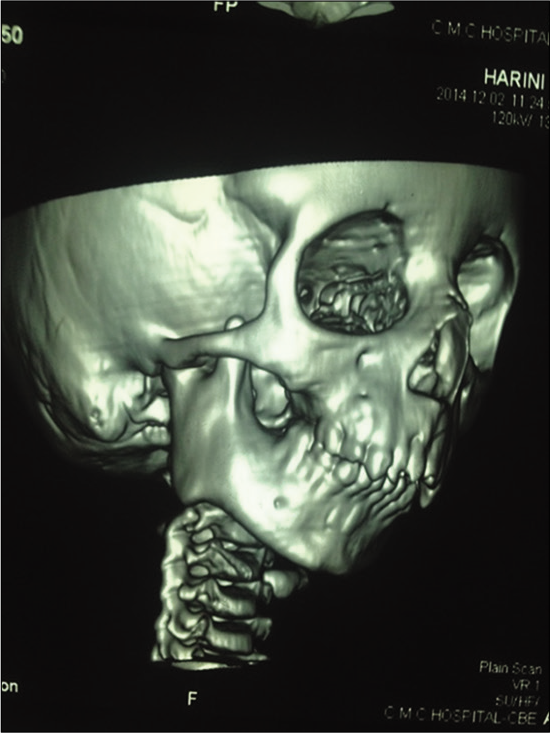
- CT scan – right side.
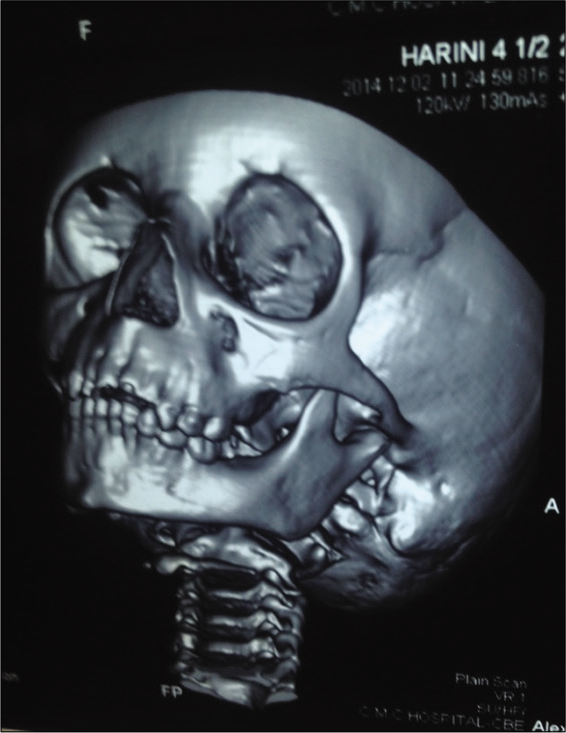
- CT scan – left side.
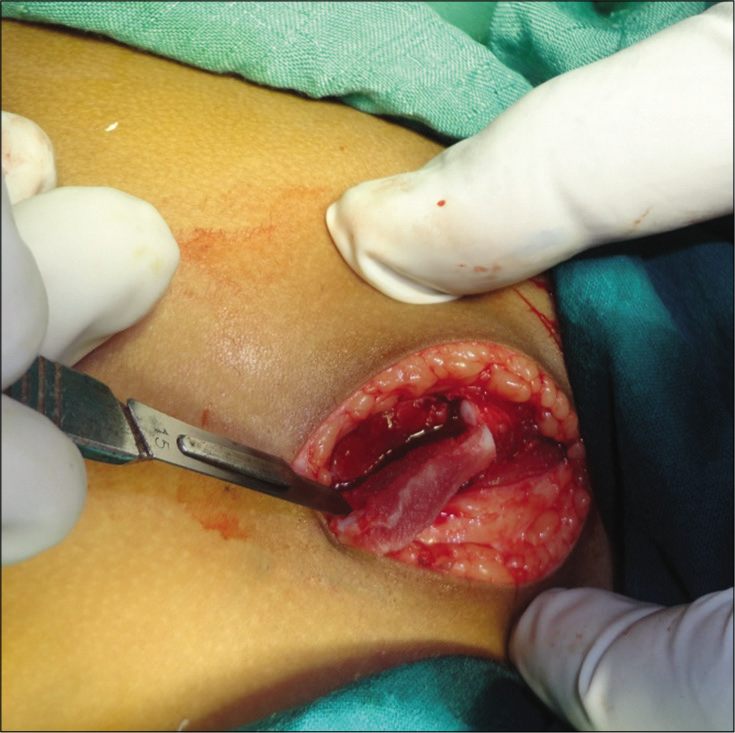
After complete clinical and radiological evaluation, a surgical treatment of gap arthroplasty at the right side was performed through the preauricular approach [Figure 8] under general anesthesia in the Department of Oral and Maxillofacial Surgery, VMSDC. After exposing and identifying the ankylosed site [Figure 9], aggressive and complete excision of the fibrous and/or bony mass was done using round bur and chisel. The excision was done till the desired mandibular movement was achieved and then the glenoid fossa was recontoured. Total TMJ reconstruction was carried out using dermis-fat graft [Figure 10] along with bilateral coronoidectomy [Figures 11 and 12].

- Pre-auricular approach.
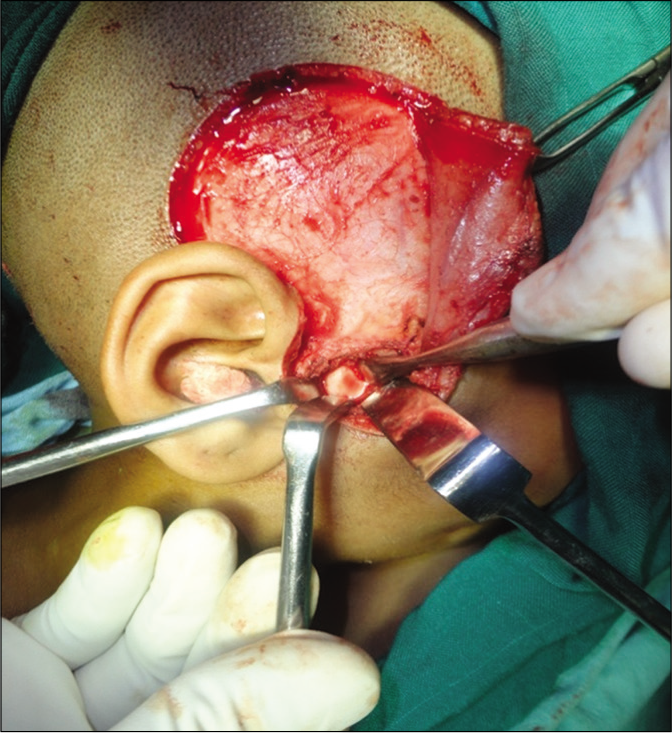
- Ankylosed TMJ.
- Dermis-fat graft.

- Coronoidectomy.

- Suturing of surgical site.
After surgery, mouth opening of 15 mm was noted and deviation of jaw to the right side has decreased [Figure 13], and on intraoral examination, the patient presented with dental caries in relation to 54, 55, 16, 64, 74, and 84 and grossly destructed teeth in relation to 65, 75, and 85 [Figures 14 and 15].

- Post-operative facial view.

- Maxillary arch.

- Mandibular arch.
To increase the mobility of the mandible, exercises for the muscles of mastication, lips, and tongue were advised. The patient was asked to chew a small rubber tube to stimulate normal mastication. Physiotherapy plays a crucial role in restoring and maintaining the normal TMJ function.
Following vigorous physiotherapy for about 3 weeks, the mouth opening increased to 3 cm [Figures 16 and 17].

- Mouth opening after physiotherapy.
- Measurement of 3 cm mouth opening.
After achieving 3 cm of mouth opening, full-mouth rehabilitation was done with extraction of 65, 75, and 85 under local anesthesia, pulpotomy in relation to 84, pulpectomy in relation to 54, 55, and 74, glass ionomer cement restoration in 26 and 36, and stainless steel crown in relation to 54, 55, and 64. Crown and loop space maintainer in relation to 75, band and loop space maintainer in relation to 65 [Figures 18 and 19], and removable functional space maintainer in relation to 53, 52, 51, 61, and 62 were given.

- Post-operative maxillary arch.

- Post-operative mandibular arch.
Psychological counseling and speech therapy were started right from the initial visit and last even after TMJ surgery.
DISCUSSION
Trauma is the most common cause for TMJ ankylosis.[9] Due to bone formation from intra-articular hematoma, limited jaw joint movement occurs.[10] Reankylosis may occur as a result of incomplete or inadequate primary reossification or inadequate jaw stretching for any reason.[11]
As reported by Dimitroulis, dermis-fat graft as an interpositional graft was used in the present case.[12] According to Movahed and Mercuri, using fat graft, the formation of fibrosis and heterotopic calcification is prevented as it acts a physical barrier.[13]
Bilateral coronoidectomy was performed in the patient to increase the mouth opening according to the protocol by Kaban et al.[2] In TMJ ankylosis, the hyperplastic ipsilateral or contralateral coronoid process impinges on the zygomatic bone and zygomatic arch causing restriction in mouth opening,[14,15] thereby by doing coronoidectomy helps in enhancing the mouth opening in TMJ ankylosis cases.
Speech and appearance contribute equally to low self-esteem in the patient. Unusual speech was the problem faced by the patient due to jaw thrusting and was eventually corrected due to effective speech therapy.[16-18] Speech, functional, and psychological therapies influenced the patient to bring about a positive attitude.
Psychological counseling was insisted as an attempt to understand the feeling of disfigurement in face during the pre-treatment and post-treatment stages using standardized questionnaires.[16-18]
CONCLUSION
TMJ reankylosis in children is a challenging problem. A careful surgical technique and a long-term physiotherapy are considered essential to achieve a satisfactory result.[19] Specialists involved in the “Inter-Disciplinary Approach” for the treatment of TMJ ankylosis helped in achieving functional efficiency, structural stability, esthetic harmony, and psychosocial competency.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Textbook of Oral and Maxillofacial Surgery (1st ed). New Delhi, India: Elsevier; 2004.
- [Google Scholar]
- A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145-51.
- [CrossRef] [Google Scholar]
- Aetiology and presentation of ankylosis of the temporomandibular joint: Report of 23 cases from Abuja, Nigeria. Br J Oral Maxillofac Surg. 2012;50:80-4.
- [CrossRef] [PubMed] [Google Scholar]
- Traumatic temporomandibular joint ankylosis: Our classification and treatment experience. J Oral Maxillofac Surg. 2011;69:1600-7.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical management of temporomandibular joint ankylosis in ankylosing spondylitis. Int J Rheumatol. 2011;2011:5.
- [CrossRef] [PubMed] [Google Scholar]
- An epidemiological study of temporomandibular joint ankylosis. Natl J Maxillofac Surg. 2012;3:25-30.
- [CrossRef] [PubMed] [Google Scholar]
- Textbook of Pedodontics (1st ed). New Delhi: Jaypee Brothers Medical Publishers Ltd; 2002.
- [Google Scholar]
- Temporomandibular joint ankylosis pattern, causes and management among a sample of Sudanese children. J Dent Craniofac Res Den Craniofac Res. 2017;2:6.
- [CrossRef] [Google Scholar]
- Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: A report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;87:166-9.
- [CrossRef] [Google Scholar]
- Ankylosis of the mandible: Analysis of 76 cases. J Oral Maxillofac Surg. 1983;41:442-9.
- [CrossRef] [Google Scholar]
- Unfavorable results intemporomandibular joint ankylosis surgery. Indian J Plast Surg. 2013;46:235-8.
- [CrossRef] [PubMed] [Google Scholar]
- The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2004;33:755-60.
- [CrossRef] [PubMed] [Google Scholar]
- Management of temporomandibular joint ankylosis. Oral Maxillofac Surg Clin North Am. 2015;27:27-35.
- [CrossRef] [PubMed] [Google Scholar]
- Oral submucous fibrosis: Its pathogenesis and management. Br Dent J. 1986;160:429-34.
- [CrossRef] [PubMed] [Google Scholar]
- Large exostosis of the mandibular coronoid process: Report of a case. Oral Surg Oral Med Oral Pathol. 1990;69:559-62.
- [CrossRef] [Google Scholar]
- Temporomandibular joint ankylosis in a child: An unusual case with delayed surgical intervention. BMC Pediatr. 2015;15:169.
- [CrossRef] [PubMed] [Google Scholar]
- TMJ ankylosis: Multidisciplinary approach of treatment for dentofacial enhancement-a case report. Case Rep Dent. 2011;2011:187580.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of temporomandibular joint ankylosis: A case report. J Can Dent Assoc. 2001;67:659-63.
- [Google Scholar]
- Temporomandibular joint ankylosis: Report of 14 cases. Int J Oral Maxillofac Surg. 2003;32:24-9.
- [CrossRef] [PubMed] [Google Scholar]






