Translate this page into:
Prosthodontic management of a partially edentulous patient with systemic sclerosis: A case report

*Corresponding author: Leoney A, Department of Prosthodontics and Crown and Bridge, GDCH, Chidambaram, Tamil Nadu, India. antony.leoney@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ramesh S, Leoney A. Prosthodontic management of a partially edentulous patient with systemic sclerosis: A case report. J Academy Dent Educ 2023;9:39-42.
Abstract
Systemic sclerosis patients have restricted mouth opening along with narrowing of the oral aperture. This situation makes the clinical procedures associated with prosthodontic rehabilitation cumbersome and challenging. Manual dexterity of the patient is affected which could lead to poor oral hygiene maintenance as well as difficulty in insertion and removal of the removable prosthesis. This case report deliberates the difficulties in rehabilitating the partial edentulous state of an early diagnosed patient with systemic sclerosis.
Keywords
Re movable partial denture
Systemic sclerosis patient
Modified impression technique
INTRODUCTION
Systemic sclerosis (SSc) is a multisystem connective tissue disease which is characterized by fibrosis of internal organs including the heart, lungs, and gastrointestinal tract and fibrosis of skin. There are two main forms: (1) SSc and (2) localized scleroderma. SSc is further divided into limited cutaneous scleroderma and diffuse cutaneous scleroderma. Limited cutaneous scleroderma was previously called CREST Syndrome (Calcinosis cutis, Raynaud’s phenomenon, esophageal dysmotility, Sclerodactyly, and Telangiectasia). The etiology of SSc is unclear, but the pathogenesis is characterized by vascular damage and an accumulation of collagen and other extracellular matrix components at involved sites. Biopsies of the skin in early stages show bundles of collagen in the lower dermis and upper subcutanium in association with perivascular and interstitial mononuclear cell infiltrates. Unregulated collagen deposition is a hallmark of this disease.
Patients with SSc typically have rapid skin thickening and visceral organ involvement. Raynaud’s phenomenon is the most common initial finding of SSc. Skin thickening of SSc patients begins in the fingers and hands in almost all patients. The neck and the face are usually the next sites to be involved. The changes begin with pitting edema that is replaced by tautness and hardening of the skin. This limits motion in affected areas. Hyperpigmentation and subcutaneous calcifications may also occur leading to retrognathia. Oral manifestation includes rigid lips and narrow oral aperture. Skin folds are lost around the mouth, giving a mask like appearance to the face. The tongue can also become hard and rigid, making speaking and swallowing difficult. Oral telangiectasia is most commonly observed on the hard palate and lips. When fibrosis involves the muscles of mastication, mandibular resorption can occur. Dental radiographic findings such as uniform thickening of the periodontal membrane, especially around the posterior teeth, are found in 10–37% of patients. Other radiographic findings include Calcinosis of the soft tissues around the jaws. Manual dexterity is limited in scleroderma patients, which decreases their ability to maintain good oral hygiene.
Oral hygiene can be complicated further if the opening is limited. Medications may reduce salivary flow rates or patients with scleroderma may have secondary Sjogren syndrome. Xerostomia results in an increased susceptibility to dental caries and candida infection. Circulating anti-nuclear auto antibodies are present in >90% of scleroderma patients. These include anti-centromere antibody (ACA), anti-topoisomerase I (anti topo-I), anti-ribonucleic acid (RNA) polymerase-I/III, and anti-Th/To 2–36. ACAs are strongly associated with slowly progressive and limited disease, whereas anti-topo I and anti-RNA polymerase I/III are found more frequently in patients with progressive and diffuse disease. Prosthodontic treatment in an edentulous patient poses problems using conventional methods, smallest available impression tray can be used.
CASE REPORT
A 45-year-old female patient reported to the department of prosthodontics with a chief complaint of missing teeth in her lower jaw front and back region for the past 1 month. She was a known diagnosed case of SSc and was under treatment for the past 2 months. Her blood report indicated a strong positive for Scl-70 antigen [Figure 1].
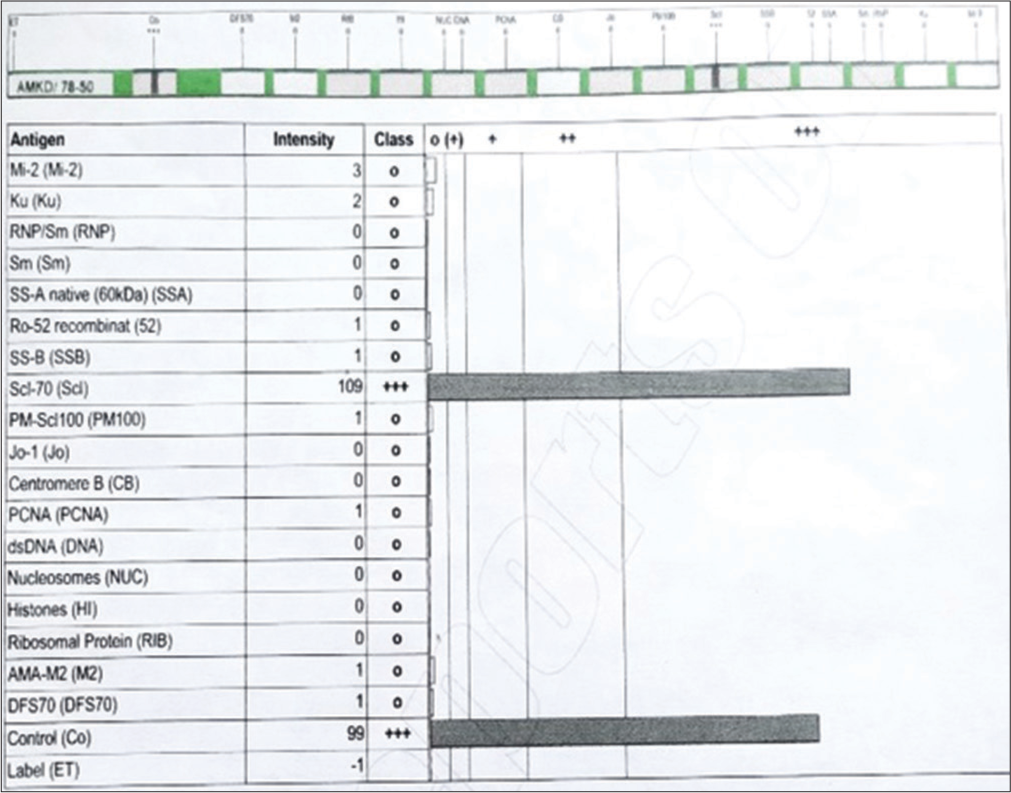
- Laboratory report of scl-70 antigen.
Extraoral examination
Her general physical examination revealed hardening and discoloration of facial skin and vertical grooving and thinning of lips causing difficulty in mouth opening. Skin discoloration and hardening were also evident in upper extremities which impairs her physical well-being [Figure 2].

- Patient extraoral photos (a) face, (b) arm, and (c) hand.
Intraoral examination
Examination reveals missing teeth in 31, 32, 36, 37, 41, and 42. Her mouth opening was about 30 mm [Figure 3].

- Intraoral image.
Preparation of denture
Impression recording was a challenging task, as the patient’s mouth opening was not adequate for the insertion of the impression trays, especially for mandibular impression. Impression was taken using the smallest available stainless steel tray using alginate [Figure 4]. Patient is asked to purse the lip and keep the lips flaccid during impression taking. Positive replica was prepared using dental stone. Clasp designing was done for better retention of denture. Baseplate adaptation, occlusal rim preparation, and teeth setting were done [Figure 5].
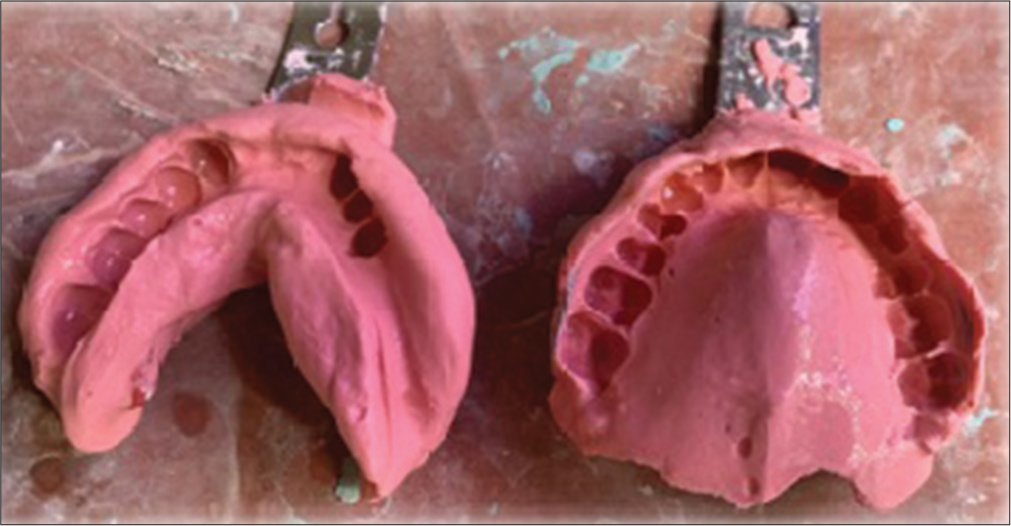
- Maxillary and mandibular impressions.
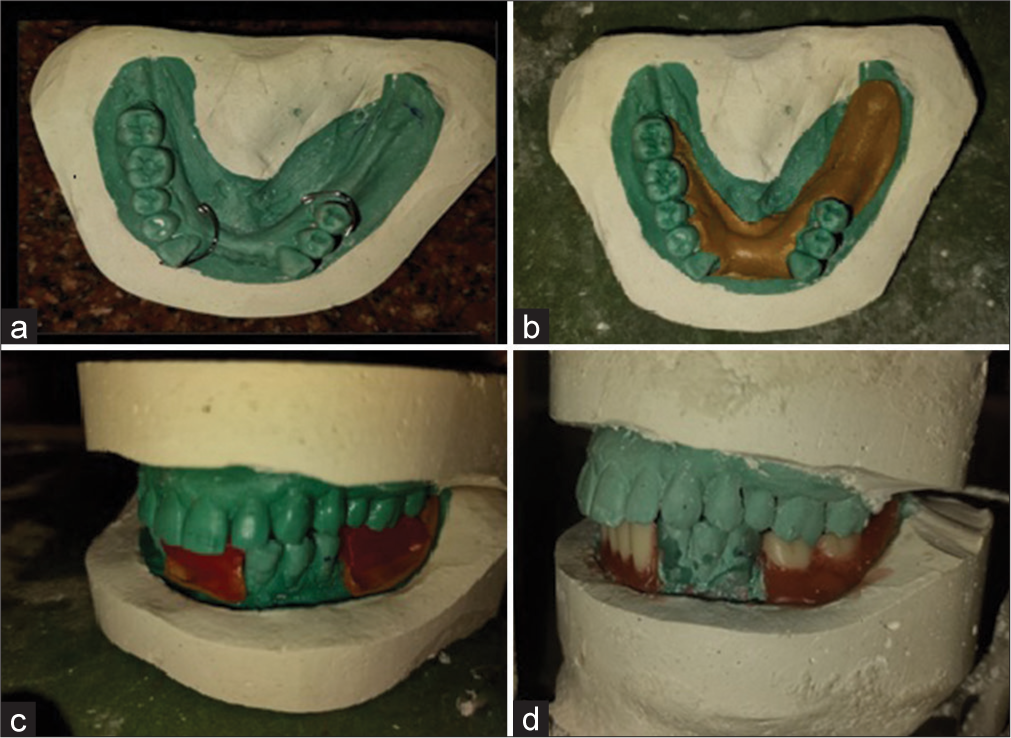
- (a) Wrought wire adaptation on cast, (b) temporary record base adaptation, (c) bite rim fabrication, and (d) teeth set-up on articulator.
Denture insertion
Denture insertion was also a challenging task due to restricted mouth opening. This article claims that not every patient with SSc requires special techniques, even a conventional interim denture can be used to rehabilitate such patients [Figures 6 and 7].

- Processed acrylic removable partial denture.

- (a) Facial view after removable partial denture (RPD) insertion and (b) intraoral view after RPD insertion.
DISCUSSION
AntiTopo I, ATA, Scl-70 are most commonly detected in patients with diffuse cutaneous SSc (dcSSc) and these patients are associated with pulmonary complications, digital ulcers, and hand disability.[1] Laboratory findings of our patient show strong positive for Scl-70 antibody. In some patients with dcSSc anti-RNA polymerase III are detected, carrying a higher risk of renal crisis.[1,2] Hypo or hyperpigmentation and telangiectasia of skin are usually found on trunk, proximity, and face giving a “mask like face” appearance.[3] In this present patient, mouth opening was restricted to 30 mm. This is in accordance with a study conducted by Marmary et al., which found that about 80% of 21 SSc patients examined were unable to open mouth beyond 40 mm.[4] Our patient did not have dental caries associated with xerostomia. This was not in accordance with surveys conducted by Marmary et al., Alarcón-Segovia et al., and Crincoli et al.[4-6]
Oral hygiene is usually poor in systemic sclerotic patients, due to decreased manual dexterity, caused by thickening of skin in proximities. Our patient was diagnosed in the early stage of the disease and was under regular treatment, thus her physical well-being was not much compromised. Fibrosis of tongue and buccal mucosa was found in patients with SS in a survey conducted by Jagadish et al.[7] Whereas our patient did not had fibrosis of tongue and buccal mucosa.
CONCLUSION
Prosthodontic management of patients with systemic sclerosis is challenging as patients have restricted mouth opening which makes impression making, denture delivery and post-denture adjustment procedures cumbersome. Modification in the conventional prosthodontic procedures will pave way for success of removable partial dentures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Severe organ involvement in systemic sclerosis with diffuse scleroderma. Arthritis Rheum. 2000;43:2437-44.
- [CrossRef] [PubMed] [Google Scholar]
- Biomarkers in systemic sclerosis: Their potential to predict clinical courses. J Dermatol. 2016;43:29-38.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic sclerosis-multidisciplinary disease: Clinical features and treatment. Reumatologia. 2019;57:221-33.
- [CrossRef] [PubMed] [Google Scholar]
- Scleroderma: Oral manifestations. Oral Surg Oral Med Oral Pathol. 1981;52:32-7.
- [CrossRef] [PubMed] [Google Scholar]
- Sjogren's syndrome in progressive systemic sclerosis (Scleroderma) Am J Med. 1974;57:78-85.
- [CrossRef] [PubMed] [Google Scholar]
- Orofacial manifestations and temporomandibular disorders of systemic scleroderma: An observational study. Int J Mol Sci. 2016;17:1189.
- [CrossRef] [PubMed] [Google Scholar]
- Oral and periodontal manifestations associated with systemic sclerosis: A case series and review. J Indian Soc Periodontol. 2012;16:271-4.
- [CrossRef] [PubMed] [Google Scholar]






