Translate this page into:
Proprioception and osseoperception in prosthodontics – A review

*Corresponding author: Leoney A, Department of Prosthodontics and Crown and Bridge, Government Dental College, Chidambaram, Tamil Nadu, India. antony.leoney@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sashi V, Leoney A, Port Louis LR. Proprioception and osseoperception in prosthodontics – A review. J Academy Dent Educ 2023;9:24-7.
Abstract
The masticatory system receives neural inputs by means of proprioception and perception. Defective proprioceptive or perceptive input results in dysfunctional or pathological conditions. The prognosis of a prosthodontic restoration depends on the integration of proprioceptive input and motor output. The absence of intradental and periodontal mechanoreception accompanying tooth loss alters the fine proprioceptive control feedback. Complete denture rehabilitation is a compromised restoration which restores function with many lacunae. In contrast to conventional dentures, implant-supported prostheses restore jaw function with improved psychophysiological discriminatory ability, oral stereognosis, and osseoperception.
Keywords
Proprioception
Mechanoreceptors
Implants
Osseoperception
INTRODUCTION
Meaning of proprioception
Proprioception (otherwise known as kinesthesia) is defined as an unconscious sense that imparts an individual with the knowledge of their body’s position and physiologic state of their joints, muscles, limbs, etc. A proprioceptive receptor is the receptor which is affected by stimuli within the tissues and organs that convey deep pressure, orientation, tension, as well as awareness to change in position and movements.[1]
Components of proprioception
The proprioceptive performance is dependent on proprioceptive information provided by the various receptors (which is the hardware component) and proprioceptive ability (which is the software component).[2,3]
PROPRIOCEPTIVE INFORMATION
The proprioceptive information is conveyed to the integration centers for processing. The proprioceptive information is gathered by receptors. The various receptors are as follows.
Joint mechanoreceptor
Mechanoreceptors of low threshold are located in temporomandibular joint (TMJ). They play a protective role in signaling movements and positions of joints,[4] for example, Free nerve endings and Golgi-Mazzoni end organs (GTOs) and Corpuscular end organs.[1]
Muscle mechanoreceptors
The major mechanoreceptors present in the muscles are GTOs. GTOs are present at the musculotendinous junction along with extra fusal muscle fibers. GTOs are involved in sensing the intramuscular tension produced during voluntary contractions (e.g., mastication). The muscle spindles transmit the sensory feedback (length and tonus of muscles) and thus act as proprioceptors.[1,4]
Mucosal mechanoreceptors
In dentulous conditions, periodontal mechanoreceptors are pivotal for precise interdental discrimination. Recently, implant-supported prostheses are replacing conventional complete dentures, but they pose the problem of activation of mucosal receptors under the prosthesis leading to proprioception. Examples of mucosal mechanoreceptors include Meissner’s corpuscules, Merkel cells, glomerular endings, free nerve endings, and Ruffini-like endings.[4]
Periosteal mechanoreceptors
Examples include complex unencapsulated endings, encapsulated endings, and free nerve endings. They are activated by the exertion of pressure on the periosteum by masticatory muscles and the mucosa.
PROPRIOCEPTIVE ABILITY
Central neural representation
There is extensive representation within the central nervous system from mechanoreceptors (cutaneous and mucosal), muscle spindles, GTOs (from jaw muscles), and mechanoreceptors (from TMJ and periodontal ligament (PDL). These representations are at various levels of the trigeminal sensory nucleus, the orofacial somatosensory afferent pathway, the primary somatosensory cortex, and the ventroposteromedial nucleus of the thalamus.[5]
Activation of periodontal sensory endings following stimuli in and around the tooth is conveyed to the trigeminal neurons in the trigeminal ganglion. Then, signals are transmitted to the ventral posterior nucleus (thalamus) and sensory cortex causing the neurosensory pathway feedback. In contrast to this in implants, there is deficiency in PDL mechanoreceptive input causing hampered peripheral feedback[6] [Figure 1].
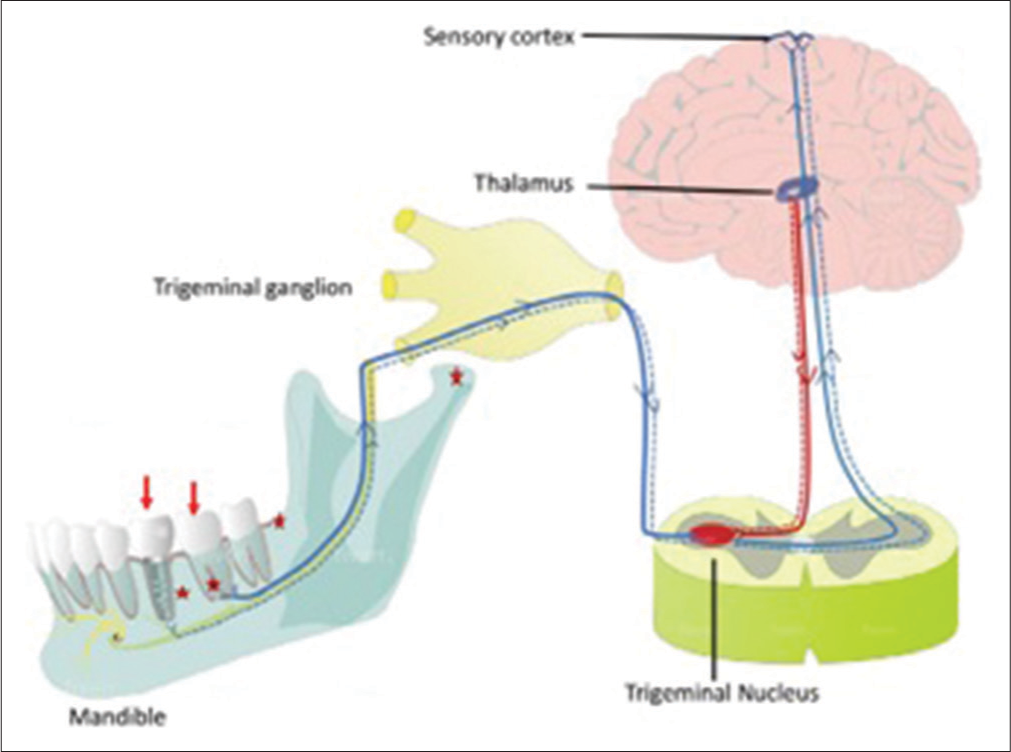
- Sensory pathway for tooth/implant stimuli (red stars)-sensory nerve endings, (blue and red solid lines) neurosensory pathway feedback.
Chewing center concept
A recent concept in masticatory control is that the mastication is regulated by a “chewing center.” Similar to the presence of respiratory center for rhythmic breathing, there is a chewing center for rhythmic mandibular movements.
The chewing center is activated by either peripheral sense organs (intraoral and extraoral sensory organs) or higher brain centers (cerebral cortex, extrapyramidal system, and midbrain-pontine nucleus). A diagram representing the somatotopic organization within the somatosensory cortex of mechanoreceptive afferent input from the surface of body is given in [Figure 2].
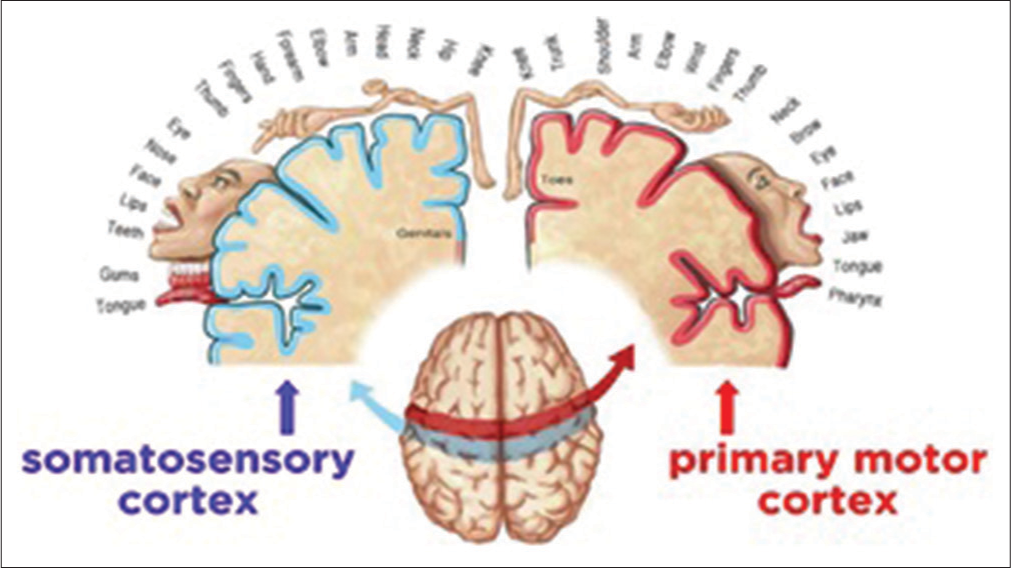
- Somatotopic organization within the somatosensory cortex and primary motor cortex.
PROPRIOCEPTION AND ITS IMPLICATIONS IN PROSTHODONTICS[1]
Teeth’s tactile sensitivity to masticatory load
Anterior teeth exhibited 10 times higher sensitivity to axial load than posterior teeth. Teeth exhibited more sensitivity to lateral load compared to axial load.
Canine response
Canines have higher proprioceptive capabilities when compared to other teeth. The last natural teeth to be lost are the canines. Retaining the canine teeth for a conventional prosthesis or overdentures to retain the sensory feedback are of great importance.
Directional sensitivity
PDL is directionally sensitive. The receptors around the teeth receive the directional stimuli. PDL showed less directional sensitivity in axial direction when compared to that of along the long axis of the teeth.
Dimensional proprioception
It can be divided into two categories: (1) Discrimination of changes in the thickness of a material and (2) determination of minimal thickness. The size judgment is established by proprioceptive sensations from the masticatory muscles and TMJ. The ability to judge texture was considerably less in majority of denture wearers when compared to dentulous patients.
Perception of oral cavity
A complete edentulous state leads to total loss of the sensory input that had been provided by the PDL. The similar sensory mechanism which maintains the mandibular posture in the infant (i.e., in the edentulous state) also maintains it in the edentulous. The sensory inputs from the TMJ and mucosal receptors compensate for the loss of tooth associated proprioception.
COMPLETE DENTURES
The resorption of basal bone and impairment in neuromuscular function, due to the reduction in the proprioceptive response resulting from teeth loss, eventually leads to denture failure. Complete denture patients reveal denture maladaptation with time due to residual ridge resorption. Patients with removable over-dentures, gaining support and retention from retained teeth or implants, have better prosthodontic outcomes. The obvious way to prevent denture problems is to save the natural dentition.[3]
OVERDENTURES
Retention of natural teeth as abutment for overdentures preserves some of the sensory input from the PDL receptors, which is more accurate when compared to the sensory feedback that is obtained from the oral mucosa. The receptors located in the periodontal membrane and muscles of mastication possess more discriminatory abilities than other tactile senses. The objectives fulfilled by the overdenture are (a) maintenance of teeth as a part of residual alveolar ridge which results in improved denture stability and retention, (b) decreased rate of alveolar bone resorption, and (c) maintenance of proprioceptive response by intact PDLs, that is, an increase in the patient’s manipulative skills in the handling the denture.[3]
OTHER TYPE OF DENTURES
Overdentures have more of biological importance, while immediate dentures fulfill mostly functional and psychological requirements that are mainly associated with immediate functional rehabilitation.
Cu-Sil like dentures is designed to preserve the existing natural teeth and the alveolar bone supporting them. They are found to increase the retention and stability of dentures. Patient’s psychologic satisfaction of retaining the natural teeth is augmented. Vertical dimension and proprioception is preserved by retained natural teeth.
OSTEOPERCEPTION AND DENTAL IMPLANTS
When a patient becomes partial or completely edentulous, there is impairment of esthetics, loss of function, and PDL loss along its mechanoreceptors. The conventional treatment choice of removable prosthesis has poor stability during normal jaw movements. It results in mastication problems and at times painful mastication, which leads to poor nutrition for the denture wearer. Dental implants are the alternative treatment options which provide better functional ability due to the tactile sensitivity ability known as osseoperception.[4,5]
DEFINITION OF OSSEOPERCEPTION
Osseoperception is described as mechanoreception when there is complete loss of a functional periodontal mechanoreceptive input and it is acquired from perioral mechanoreceptors that provide mechanosensory information for kinaesthetic sensibility of oral cavity.
THEORIES OF OSSEOPERCEPTION[4,5] (BASED ON NEURAL INPUTS DERIVED FROM JAW MOVEMENTS)
Theory 1: After extraction, periodontal receptors persist within the bone (Linden RWA, Scott BJJ, 1989)
Theory 2: Reinnervation in relation with controlled forces directed to implants (Bonte et al., 1993)
Theory 3: TMJ receptors replace the PDL receptors of natural teeth (Klineberg and Murray, 1999)
Theory 4: Periosteum could be the origin of proprioceptive responses (Van Steenberghe, 2000)
Theory 5: Bones adjacent to implants contain nerve fibers (Weiner et al., 2004).
OSSEOPERCEPTION AND ITS CLINICAL IMPLICATION [6]
The concept of osseoperception by osseointegrated implant-supported prosthesis helps to restore the habitual masticatory physiologic function, despite the absence of periodontal mechanoreceptors
The inability to attain optimum osseoperception might cause failure of implant due to overloading
The osseoperception and implant healing are affected by oral parafunctional activities such bruxism, night grinding, etc.
By immediate placement of implant and loading protocol, a positive effect on neurosensory fiber content was observed.
CONCLUSION
Proprioception and perception act as inputs to program and monitor the motor responses which act as the outputs. PDL sensory nerve endings are pain and pressure receptors which combine with the proprioceptive input from various receptor sources to control the mandibular motor function and its physiologic resting position. Complete edentulism leads to the total loss of proprioception, distinct discrimination, directional sensitivity, dimensional proprioception, and tactile sensitivity. The merger of proprioceptive feedback and motor responses is the core of the success or failure of prosthodontic treatment. The osseoperception phenomenon in dental implants helps in restoring the sensory feedback pathway, thereby promoting implant success rates.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Oral perception and proprioception: A review of the literature and its significance to prosthodontics. J Prosthet Dent. 1972;28:215-30.
- [CrossRef] [PubMed] [Google Scholar]
- Reflexes elicitable in jaw muscles and their role during jaw function and dysfunction: A review of the literature. Part I: Receptors associated with the masticatory system. Cranio. 1987;5:139-51.
- [CrossRef] [PubMed] [Google Scholar]
- Oral proprioception for prevention and preservation. Res Rev J Dent Sci. 2014;2(Supple 1):42-6.
- [CrossRef] [Google Scholar]
- Osseoperception: An implant mediated sensory motor control-a review. J Clin Diagn Res. 2015;9:ZE18-20.
- [CrossRef] [PubMed] [Google Scholar]
- Osseoperception: Sensory function and proprioception. Adv Dent Res. 1999;13:120-9.
- [CrossRef] [PubMed] [Google Scholar]
- Osseoperception following dental implant treatment: A systematic review. J Oral Rehabil. 2022;49:573-85.
- [CrossRef] [PubMed] [Google Scholar]







