Translate this page into:
Prevalence of temporomandibular joint disorders and its association with stress among dental students in Davangere city – A cross-sectional survey

*Corresponding author: B. Sapna, Department of Public Health Dentistry, Bapuji Dental College and Hospital, Davangere, Karnataka, India. sapnaprasanna@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chinthalapalli S, Sapna B, Gujjar VP, Sulthana DS, Chalamala N, Neha NC, et al. Prevalence of temporomandibular joint disorders and its association with stress among dental students in Davangere city – A cross-sectional survey. J Academy Dent Educ. 2024;10:71-5. doi: 10.25259/JADE_13_2023
Abstract
Objectives:
Dental students are exposed to some complex experiences that predominantly lead to stressful situations and expose them to temporomandibular disorders (TMDs).Aim: The aim of this study was to determine the prevalence of TMD and how it relates to stress among dental students.Study Setting and Design: A cross-sectional survey was carried out among 283 undergraduate dental students, who consented to participate across all academic levels.
Material and Methods:
TMD was evaluated using the Diagnostic Criteria for TMDs Axis-I and Axis-II methodology. In Axis-I, screening and clinical examinations of TMD, and in Axis-II, stress as one of the psychosocial risk factors of TMD is evaluated using the modified dental environment stress scale (DESS).
Results:
The overall prevalence of TMD was 61.2 %. Headache followed by clicking, pain on clicking, difficulty in mouth opening, and jaw locks were the most commonly reported symptoms. On clinical examination, clicking was the most common TMD sign, followed by temporomandibular joint pain. Among the various TMDs, the most prevalent TMD was disc displacement followed by myofascial pain dysfunction syndrome. Females were slightly more affected by TMDs than males. TMDs were more common among the final year dental students followed by interns (house surgeons). Further, participants with TMD symptoms and signs had significantly higher mean DESS scores than others.
Conclusion:
It has been demonstrated that dental students, particularly those enrolled in clinical programs, have a higher chance of acquiring TMDs, which has been strongly linked to elevated levels of stress.
Keywords
Prevalence
Temporomandibular joint disorders
Dental students
Diagnostic criteria for temporomandibular joint disorder
Dental environment stress scale
INTRODUCTION
Temporomandibular disorders (TMDs) hold great significance as a health issue affecting many in today’s society.[1,2] This category involves various clinical conditions impacting the masticatory muscles, the temporomandibular joint (TMJ), and nearby tissues, either separately or collectively. TMD is linked to several factors such as stress, bruxism, malocclusion, emotions, trauma, poor posture, and arthritis.[2] Stress seems to have a stronger impact on students compared to the general population.[3,4]
Dental school is known for its rigorous demands.[5] This is mainly due to the numerous skills required by dental students, many of which are associated with heightened stress levels. These competencies include intellectual knowledge, practical abilities, and interpersonal skills. The primary stressors for dental students revolve around meeting academic criteria, developing manual dexterity, mastering clinical strategies, undergoing exams, the fear of failing (particularly in front of parents), job anxieties, and financial limitations.[6] Furthermore, some dental students may encounter the challenge of being geographically distant from their families, potentially complicating their circumstances as they cannot always depend on familial support.[5]
In a study conducted by Kaushal et al.,[3] stress was found to significantly increase the likelihood of TMDs among dental students.[3] To prevent TMD in dental students, it is crucial to proactively recognize stress levels and alleviate their impact. No evidence in the literature shows stress-related TMJ disorders among dental students in Davangere City. Thus, a cross-sectional survey was initiated to evaluate the prevalence of TMD and its correlation with stress levels among dental students in Davangere City.
MATERIAL AND METHODS
Study design and duration
This was a descriptive cross-sectional research project approved by the Institutional Ethics Committee (BDC/Exam/509/2019-20). The research took place from December 2019 to November 2020, spanning almost an entire year.
Study population
All dental students who voluntarily gave their informed consent to participate (283), ranging from 1st year Bachelor of Dental Surgery (BDS) to interns, were included in the study. Students were not pressured to partake in the study. Those with dental pain, head and neck trauma, diagnosable psychological or neurological conditions, or receiving treatment for such conditions were excluded from the study.
Training and calibration of examiners
Two specialists from the Department of Oral Medicine and Radiology were chosen for clinical examinations following the Diagnostic Criteria for TMDs (DC/TMD) protocol. Before the study, all examiners underwent a self-directed training session based on the INFORM methodology.[7]
Assessment of TMD
The DC/TMD Axis-I and Axis-II protocols were employed.[8] In Axis-I, screening and clinical examinations were conducted for TMDs, while Axis-II evaluated stress as a psychosocial risk factor for TMDs using the modified dental environment stress scale (DESS).
Data collection
The DC/TMD symptom questionnaire and the DESS questionnaire were distributed through a web-based survey link to all dental students (388). A 73% acceptance rate was observed, where 283 students consented to participate and responded to the questionnaire and these students were then clinically examined at the Department of Oral Medicine and Radiology.
Data analysis
Data were entered into a Microsoft Excel sheet and analyzed using the Statistical Package for the Social Sciences v.21. Descriptive statistics were constructed using frequency and percentages. Inferential statistics by applying the Chi-square test for categorical data and the student t-test for continuous data.
RESULTS
The present cross-sectional research was to determine the prevalence of TMDs among dental students and the relationship between those conditions and stress. Two hundred and eighty-three dental students, ranging from I BDS to interns, took part in the study. Participants’ ages ranged from 17 to 25, with a mean age of 19.4 ± 2.3 years with females constituting nearly 77.4% (n = 219) of the study population. About 29.3% and 23.7% of subjects were from 3rd and final-year BDS, respectively.
TMD symptoms
Around 134 (61.2%) of individuals reported having at least one TMD symptom, according to the screening of subjects with the criteria of the DC/TMD Axis-I. In addition, the most prevalent TMD symptom was a headache (53.7%), which was followed by clicking (35.1%), pain from clicking (28.9%), and difficulty opening the mouth (11.2%). Among the students, just 2.2% reported having jaw locks [Figure 1].
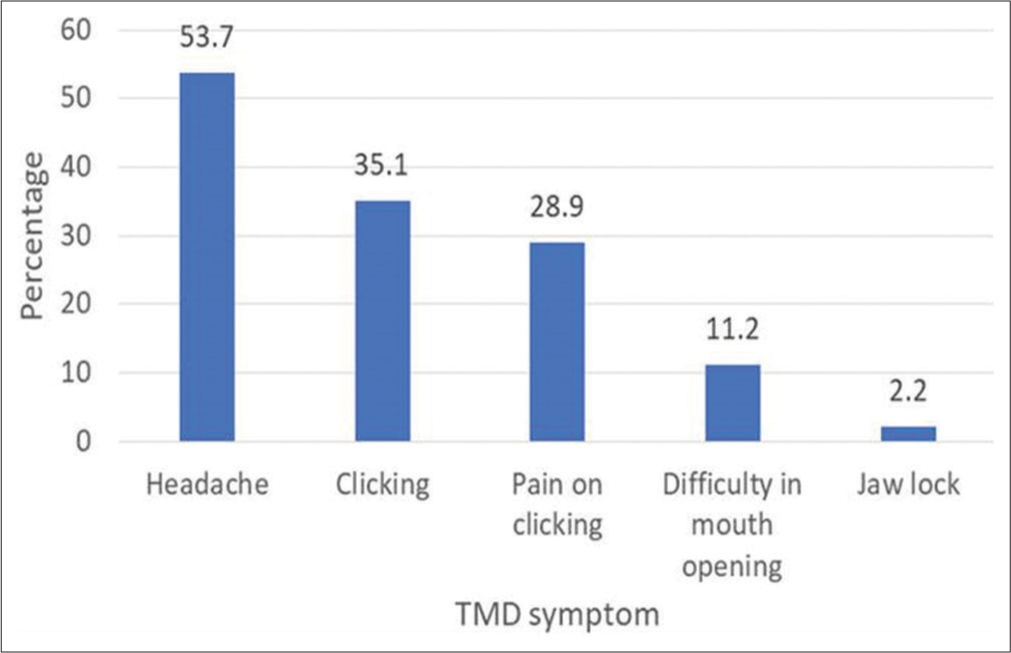
- Prevalence of temporomandibular disorder (TMD) symptoms.
TMD signs
On clinical examination, about 78 (27.2%) of the study participants showed TMD signs. Clicking (40.3%) was the most common TMD sign followed by TMJ pain (28.6%) [Figure 2].
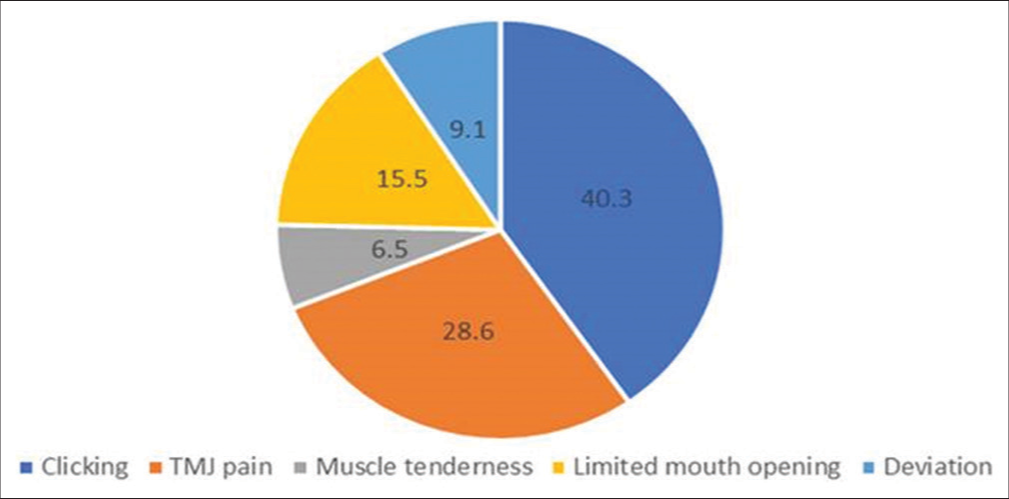
- Prevalence of temporomandibular disorder signs temporomandibular joint (TMJ).
TMJ disorders
The most common type of TMD was identified by combining the favorable results of the symptom questionnaire and clinical evaluation. TMD diagnosed was disc displacement at 69.2%, followed by myofascial pain dysfunction syndrome (MPDS) among 26.9% and both disc displacement and MPDS were seen in 3.9% of those affected. Table 1 shows the gender-wise distribution of TMDs.
| Gender | Type of TMD in n (%) | ||||
|---|---|---|---|---|---|
| Disc displacement (54) | MPDS (21) | Disc displacement with MPDS (3) | χ2 (df-2) | P-value | |
| Male | 8 (14.8) | 3 (14.2) | 1 (33.3) | 0.7754 | 0.678 |
| Female | 46 (85.2) | 18 (85.8) | 2 (66.7) | ||
TMDs: Temporomandibular disorders, MPDS: Myofascial pain dysfunction syndrome
When TMD prevalence was compared with the year of study, TMDs were more common among students of IV BDS followed by interns and least affected, which were I BDS students but this variation was not statistically significant (P = 0.075) [Figure 3].
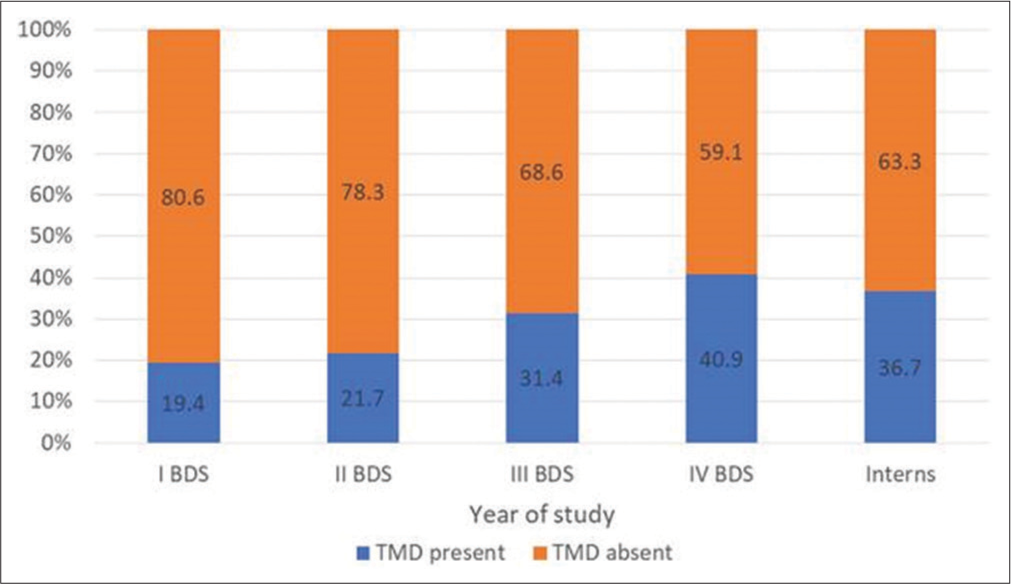
- Prevalence of temporomandibular disorders (TMD) according to the year of study.
Stress measured by DESS and its association with TMD
The total DESS scores ranged from 7 to 49. On comparing the mean DESS score according to gender, females had higher mean DESS scores than males (P = 0.015). It was not found to be statistically significant.Further, those participants who had TMD symptoms and signs and were diagnosed with TMDs had significantly higher mean DESS scores than those without them and were found to be highly significant [Table 2].
| Variables | Mean DESS score | SD | P-value |
|---|---|---|---|
| Gender | |||
| Male | 31.1 | 3.1 | 0.015 |
| Female | 32.6 | 4.6 | |
| TMD signs | |||
| Present | 34.2 | 1.5 | <0.001** |
| Absent | 30.1 | 4.1 | |
| TMD symptoms | |||
| Present | 33.5 | 5.2 | <0.001** |
| Absent | 27.6 | 1.2 | |
| TMDs | |||
| Present | 32.1 | 3.5 | <0.001** |
| Absent | 29.7 | 2.6 |
DISCUSSION
TMD is a complicated ailment that presents with several challenges.[8] According to Schwartz, temporomandibular pain dysfunction syndrome is mostly a symptom complex that affects people in their middle or younger years. It is frequently witnessed in the female population in the second to fourth decade. The following are indicative of a TMJ disorder: discomfort in the ears and preauricular region when opening/closing the jaw or chewing; clicking, popping, or grating noises; tenderness in the TMJ; reduced mouth opening; stiff or painful neck and shoulder areas. A list of other symptoms and indicators includes a lethargic countenance, challenges with biting, facial swelling on one side, toothache, headache, light-headedness, hearing problems, and tinnitus or ringing in the ears. The development of TMD and oral parafunctional disorders is attributed to both systemic and local factors, with stress and heightened psycho emotional activity being highlighted as significant psychological factors in some studies.[3,9,10]
TMD is greatly influenced by stress, which holds a crucial position in its development. The impact of this factor is particularly significant among the student population. Stressors such as the pressure of receiving a quality education, uncertainty about the future, limited financial resources, being away from home, and adapting to a foreign environment are just a few examples. In addition, students face various challenges related to social, emotional, physical, and family issues.[3] Several studies have consistently demonstrated that dental education is highly stressful for students. These findings have been observed across different countries, academic institutions, and educational programs.
Using a self-reported questionnaire, this study examined the prevalence of TMJ conditions among dental students and its correlation to stress. Among the study group, 78 students were found to have at least one symptom. Headache was the most common symptom, followed by clicking, pain on clicking, and trismus and lockjaw. This follows the study conducted by Kaushal et al. in 2017 and Ahuja et al. in 2018.[3,11]
On evaluating the TMD signs, 38 students showed TMD signs, of which clicking was the most common, followed by TMJ pain, which is under the study conducted by Chaurasia et al. in 2021.[10] The present study outlines a major disproportion between the genders, showing females are more susceptible to TMD disorder than males. Disc displacement was the most common TMD (69.2%) followed by MPDS. According to international research on 85,052 individuals from 17 countries, 62% of women and 38% of men have TMD. Similar research on student populations found that the proportions for men and women were 65% and 35%, respectively. Milam[12] and Manfredini[13] found that there was a considerable female majority (9:1); however , Bonjardim et al.[14] found that the proportion of women with TMD (57.43%) was larger than that of men (42.11%). This may be brought on by changes in hormone levels, biological variations, social position, or higher sensitivity to pain in women.
TMD prevalence was found to be comparatively higher in the final years followed by interns. Sekhon et al.[6] related investigations found that the most stressful factors were clinical and patient requirements. Examination pressure, grade anxiety, and failure-related worry were listed as some of the top stresses. It is thought that bad behaviors such as clenching, bruxism, and even excessive gum chewing are brought on by high levels of stress. These trigger muscular overuse, exhaustion, and spasms, which then cause pain.[8]
The mean DESS score was found to be higher in females (32.6 ± 3.1) compared to males (31.1 ± 4.6), indicating females were feeling more stressed than males. However, the gender difference was not statistically significant. With higher estrogen levels and a greater susceptibility to stress, females were frequently impacted more than men. Similar findings were discovered in the research conducted by Kaushal et al. in an institution in Indore city.[3]
The present study showed that individuals with TMD signs, TMD symptoms, or the presence of TMDs had higher mean DESS scores and it was found to be statistically significant (P< 0.001) as compared to people without TMDs. According to psychological theory, emotional issues cause muscles to become overactive. Due to its close connection to the limbic brain, the extrapyramidal gamma motoric system, which regulates muscle hyperactivity, is extremely susceptible to emotional influences. Local ischemia hypoxia caused by prolonged muscular stimulation and lactic acid accumulation is the cause of pain.
Considering everything mentioned above, we can deduce that the exact root cause of TMD is still unknown. However, our study confirms stress as one of the main etiological elements. The tiny sample size of this study, which only included dentistry students from one region, was one of its primary weaknesses. Future research should therefore be done with a larger sample size and a diverse group of students.
CONCLUSION
The study sheds light on the significant association between stress and TMD among dental students. The findings emphasize the need for proactive stress management strategies to mitigate TMD risks among this group. There is a call for the implementation of effective support systems within dental education to address these stress-related challenges properly. This research can serve as a foundation for larger, more diverse studies in the future to gain deeper insights into this important health issue among dental students.
Awarded the best scientific paper
The paper was presented by the first author at the 73rd Indian Dental Conference held on 23rd-26th January 2020 at Kovalam, Thiruvananthapuram and won the best scientific paper in the students and intern category in the lighthouse hall session.
Acknowledgments
We would like to thank the faculty and postgraduate students of the Department of Oral Medicine and Radiology, Department of Public health dentistry for providing permission and expertise to carry out the study. We would like to acknowledge the BDS students of all academic levels for their participation. We would like to thank the institution’s college authority and research cell for their motivation to engage in undergraduate research activities.
Ethical approval
The authors declare that they have taken the approval from the Institutional Ethics Committee and the approval number is BDC/Exam/509/2019-20.
Declaration of participants consent
The authors certify that they have obtained all appropriate participants consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary material available online
https://dx.doi.org/10.25259/JADE_13_2023
Financial support and sponsorship
Nil.
References
- Prevalence and correlation between TMD based on RDC/TMD diagnoses, oral parafunctions and psychoemotional stress in Polish university students. Biomed Res Int. 2014;2014:472346.
- [CrossRef] [Google Scholar]
- The incidence of temporomandibular joint disorders among dental students in Aljouf University, KSA. Int Innov J Med Med Sci. 2015;2:5-1.
- [Google Scholar]
- Prevalence of temporomandibular disorders in dental students: A survey in Indore city. Int J Appl Dent Sci. 2018;4:273-7.
- [Google Scholar]
- Prevalence of psychological distress in university students--implications for service delivery. Aust Fam Physician. 2008;37:673-7.
- [Google Scholar]
- Stressful life events of dental students and salivary immunoglobulin A. Int J Immunopathol Pharmacol. 2004;17(2 Suppl):49-56.
- [CrossRef] [Google Scholar]
- Perceived sources of stress among dental college students: An Indian perspective. Eur J Gen Dent. 2015;4:121-6.
- [CrossRef] [Google Scholar]
- Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group. J Oral Facial Pain Headache. 2014;28:6-27.
- [CrossRef] [Google Scholar]
- Evaluation of temporomandibular disorders among dental students of Saudi Arabia using diagnostic criteria for temporomandibular disorders (DC/TMD): A cross-sectional study. BMC Oral Health. 2021;21:211.
- [CrossRef] [Google Scholar]
- Assessment of stress level among dental school students: An Indian outlook. Dent Res J (Isfahan). 2011;8:95-101.
- [Google Scholar]
- Temporomandibular disorders in North Indian population visiting a tertiary care dental hospital. Natl J Maxillofac Surg. 2020;11:106-9.
- [CrossRef] [Google Scholar]
- Study of stress-induced temporomandibular disorders among dental students: An institutional study. Natl J Maxillofac Surg. 2018;9:147-54.
- [CrossRef] [Google Scholar]
- Pathogenesis of degenerative temporomandibular joint arthritides. Odontology. 2005;93:7-15.
- [CrossRef] [Google Scholar]
- Research diagnostic criteria for temporomandibular disorders: a systematic review of axis I epidemiologic findings. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:453-62.
- [CrossRef] [Google Scholar]
- Association between symptoms of temporomandibular disorders and gender, morphological occlusion, and psychological factors in a group of university students. Indian J Dent Res. 2009;20:190-4.
- [CrossRef] [Google Scholar]






