Translate this page into:
Paget’s Disease in Maxilla – a Case Report
*Author for correspondence
This article was originally published by Informatics Publishing and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Paget’s disease is a disorder of bone metabolism causing excessive bone remodeling which is usually seen in elderly patients. A typical case of maxillary involvement along with the craniofacial clinical and radiographical findings is presented.
Keywords
Disorder
Diagnosis
Radiology
Medicine
Surgery
1. Introduction
Paget’s disease, which is characterized by excessive and abnormal remodeling of bone, is a common disorder in middle-aged and elderly patients. The excessive remodeling gives rise to bones that are extensively vascularized, weak, enlarged and deformed with subsequent complications (Rajendran, 2009). This condition was initially named osteitis deformans by Sir James Paget, who believed the disease was caused by chronic inflammation. The affected patients may complain of pain, deafness or blindness due to cranial nerve compression. Alveolar ridge expansions take place in cases when the facial skeleton involving the maxilla and mandible is affected.
2. Case Report
A 54 year old female patient from Salem came to our OP with the complaint of swelling, pain and pus discharge from the right upper back tooth region of 6 months duration. Upon history taking, we found the patient had diabetes of 3 months duration and was under medication. She had undergone extraction of teeth and dental prosthetic rehabilitation 6 months ago. The personal history and family history were unremarkable. On extraoral clinical examination, extensive maxillary prognathism which was asymmetrical was seen (Figure 1). Intraorally, the patient had a diffuse bony expansion of the upper jaw which was tender on palpation (Figure 2). Sinus opening with pus discharge was present in the anterior region. Orthopantomogram (OPG) and lateral and antero-posterior skull radiographs showed irregular diffuse radiopacities scattered in maxilla and cranium (Figure 3) and hypercementosis, loss of lamina dura with altered bony trabeculation. Multiple osteolytic and osteosclerotic areas with generalized loss of cortical bone giving a cotton-wool appearance was seen. The patient was psychologically affected by her appearance and desired a surgical correction. Therefore, the patient was advised for multiple extractions and osseous recountouring of jaw which was done under local anesthetic in two stages. Prophylactic antibiotics were commenced prior to surgery.

- Patient diagnosed with Paget’s disease with enlargement of maxilla.

- Intraoral examinations showing diffuse bony lesion on both the labial and palatal surface of maxillary jaw. (a) (b)
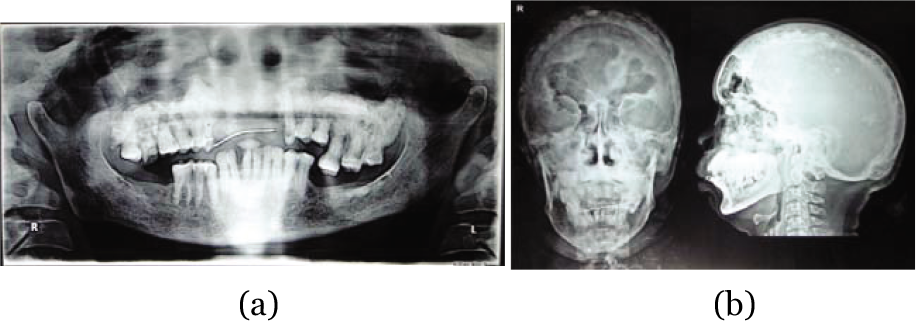
- (a) Diffuse osteosclerotic images in (a) OPG (b) AP and Lateral view.
3. Discussion
Prevalence of Paget’s disease is reported to be between 0.01% and 3% in patients above the age of 40 (Barnett & Elfenbein, 1985), increasing to 10% in patients above the age of 70 (Monteiro & Rout, 2007). The cause of Paget’s disease is unknown. There is a strong genetic component, and 15%–20% of those affected have a first-degree relative with the disease (Siris, Ottman, Flaster, & Kelsey, 1991). The maxilla is more commonly affected than the mandible. Oral manifestations of the disease include enlargement of the alveolar ridge resulting in separation of the teeth, flattening of the palate, malocclusion and pulpal calcification (Smith, & Eveson, 1981). It has been stated by many authors that bone involved in Paget’s disease is highly susceptible to infection when exposed to the oral flora (Greenberg, 2003). Dental extractions tend to be more difficult due to the hypercementosis or ankylosis of the tooth which results in a slower healing of the extraction site. A significant number of patient develop osteomyelitis secondary to the locally infected extraction sites (Woo, & Schwartz, 1995). Paget’s disease is usually asymptomatic and does not require treatment. High doses salicylates have been used for their analgesic and anti-inflammatory properties; in addition they retard collagen production and reduce hydroxypro-line excretion in pagetic patients. However, if a patient with Paget’s disease develops osteomyelitis, the treatment becomes more complex. Early management for osteomyelitis involves various maneuvers to limit the spread of the infection and allow the host to begin the process of sequestration of the devitalized bone (Brady, Roser, & Sapp, 1979). Administration of antibiotics to limit the spread of infection along with surgical decortications and the judicial extraction of teeth in order to establish drainage tracts and therefore decompress the tissue (Brady, Roser & Sapp, 1979). Treatment for Paget’s disease includes medication to help regulate bone remodeling, medication to relieve pain, physical therapy and surgery. Bisphosphonates are the first-choice treatment to regulate bone growth. They work by controlling the cells that absorb old bone (osteoclast cells), which means the bone regeneration process should return to normal (Paget’s Disease-Treatment, 2012, para. 17). A type of bisphosphonate called risedronate has proved to be effective in treating Paget’s disease and is usually recommended. Calcitonin used to be a common treatment for Paget’s disease, but is only used in certain circumstances now (Paget’s Disease-Treatment, 2012, para. 17). For instance, if the patient has hypocalcaemia, calcitonin is recommended over bisphosphonates as bisphosphonates can lower the calcium levels further. Surgery is usually only used if Paget’s disease causes further problem, such asbone deformities, where procedures such as osteotomy performed according to patient’s necessity.
4. Conclusion
Although Paget’s disease is not a highly prevalent condition, it is essential for a dental practitioner to know the features and dental manifestations of this disease and to be able to identify and diagnose effectively. It is also important to create a proper treatment plan, in which both the health and the aesthetic concern of the patient to be taken into consideration.
5. Acknowledgement
The author wish to thank Prof. Dr. Reena John for support and guidance to prepare this manuscript and Dr. Rethish Elangovan for encouragement along with providing informative materials and references.
References
- (1985) Paget’s disease of the mandible–a review and report of a case. Dental Traumatology. ;1:39-42.
- [Google Scholar]
- (1979) Osteomyelitis of the mandible as a complicating factor in Paget’s disease of bone. The British Journal of Oral Surgery. ;17:33-42.
- [Google Scholar]
- (2007). Multiple root resorption as a presenting sign of Paget’s Disease of bone. Journal Compilation 2008 Blackwell Munksgaard. Oral Surgery. ;1:53-55.
- [Google Scholar]
- (2012). NHS Choices. 2013. Retrieved Nov 8. from www.nhs.uk/Conditions/Pagets-disease/Pages/Treatment).aspx
- [Google Scholar]
- (1991) Familial aggregation of Paget’s disease of bone. Journal of Bone and Mineral Research. ;6:495-500.
- [Google Scholar]
- (1981) Paget’s disease of bone with particular reference to dentistry. Journal of Oral Pathology. ;10:233-247.
- [Google Scholar]
- (1995) Unusual presentation of the Paget’s disease of maxilla. British Journal of Oral and Maxillofacial Surgery. ;33:98-100.
- [Google Scholar]






