Translate this page into:
Oral health status and pattern of tobacco use among Tuberculosis patients

*Corresponding author: Sandeep Prakash Narwane, Department of Pharmacology and Dr. BVP Rural Medical College, PIMS, Loni, Maharashtra, India. drsandeepnarwane1984@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kunkulol TR, Viragi PS, Kunkulol RR, Narwane SP. Oral health status and pattern of tobacco use among Tuberculosis patients. J Academy Dent Educ. 2024;10:76-80. doi: 10.25259/JADE_22_2023
Abstract
Objectives:
Our study aimed to assess the oral health status and pattern of tobacco use among Tuberculosis (TB) tobacco patients visiting a tertiary care hospital.
Material and Methods:
The study was conducted on 100 TB patients using tobacco and undergoing anti-tubercular therapy, who were willing to participate in the study and met the inclusion and exclusion criteria. Demographic profiles, oral examination findings, and data related to tobacco use were recorded.
Results:
The most common age group of TB tobacco patients was between 61 and 70 years. Red/white patches were observed in 70 patients, with the most common site being buccal mucosa of the oral cavity. Seventy-four patients used smokeless tobacco, among which 38 were chewing tobacco, 29 used tobacco mishri, and 7 used gutka. Peer pressure was found to be the most common factor responsible for the start of tobacco use.
Conclusion:
The study highlights the need for intervention strategies for tobacco use among TB patients to improve their oral health status.
Keywords
Tuberculosis
Tobacco
Oral health
Smokeless
Oral examination
INTRODUCTION
Tuberculosis (TB) disease continues to represent a global threat. Several risk factors play a key role in the disadvantaged status. One of the most important risk factors is tobacco addiction, which may be smoked or smokeless tobacco (SLT).[1,2] In India, over 2.8 million TB cases were reported,[3] and about 267 million adults were using tobacco.[4] Tobacco is one of the important drivers of TB epidemic.[5,6]
The World Health Organization estimated 1.35 million deaths due to tobacco use in India.[5] India is a developing country, and tobacco smoking is becoming the popular form of tobacco consumption in rural and urban populations.[6]
There is strong evidence that tobacco use has numerous negative effects on the oral health of TB patients, for example, staining of teeth and dental restorations, reduction of the ability to smell and taste, development of oral diseases such as smokers’ palate, smokers’ melanosis, and coated tongue.[7] Even though dental caries has a multifactorial etiology, there is a suggestive relationship between tobacco use and dental caries incidence.[7]
With this above background, it was thought prudent to assess the oral health status and pattern of tobacco use among TB-tobacco patients visiting directly observed therapy shortcourse (DOTS) center of tertiary care hospital.
MATERIAL AND METHODS
The research plan, the materials (or subjects), and the methods used should be described. An explanation of how the disease was confirmed and the controls used must be included, as well as the details of the data obtained and how it was analyzed.
It was a descriptive cross-sectional study conducted in patients diagnosed with TB on anti-tubercular therapy.
Ethics
The study protocol was designed in accordance with the Declaration of Helsinki.[8] Prior approval from the Institutional Ethics Committee (No: PIMS/RMC/IEC-UG-PG/2022/127 dated 17/02/2022) was taken before the initiation of the study. The patient’s identity was kept confidential.
Study design
All the patients of either gender diagnosed with TB on anti-tubercular therapy visited the DOTS center between January 2022 and June 2022 using tobacco and willing to participate in the study were included in the study. Patients with a history of major systemic problems/syndromes, psychiatric disorders, learning disability, congenital oral disorders, and oral carcinomas and oral disorders already under dental treatment were excluded from the study.
Patients satisfying the selection criteria were enrolled for the study. All the patients were explained about the entire study protocol and written informed consent was taken.
All the eligible patients were assessed for demographic profile, oral examination (presence of red or white patches, ulcers, caries, stains, and lesions) was done by the investigator and findings were recorded in the case record form, which was recorded in a well-structured case record form. The detailed data related to tobacco use was recorded in the case record form. The following variables were recorded type of tobacco used, products used, and frequency of use. Age at which tobacco use began, contributing factors responsible for its use. Details about knowledge attitudes and practices related to oral hygiene were recorded using questionnaires. The questionnaire consisted of questions related to oral hygiene practices such as brushing, flossing, use of tooth powder or paste or any other modality for cleaning the oral cavity and teeth, and frequency of cleaning. The questionnaire was pre-validated for content by experts in dental medicine. It was translated and back translated as well as tested on ten samples before its use for the study.
Statistics
Taking into consideration 224 TB active TB patients with 60% prevalence of tobacco use among TB patients, the sample size calculated was n = 93 at 80% confidence level, which was rounded up to 100.
All the variables were analyzed using descriptive statistics, including mean, frequency, and proportion. Microsoft Excel 2019 was used for data entry and analysis.
RESULTS
One hundred patients diagnosed with TB on anti-tubercular therapy visited the DOTS center between January 2022 and June 2022 consuming tobacco. Seventy-four patients were male, and only 26 patients were female in the study.
Figure 1 shows that the most common age group of TB-tobacco patients in the study was in between 61-70 years (n=24), followed by 71-80 years (n=18).
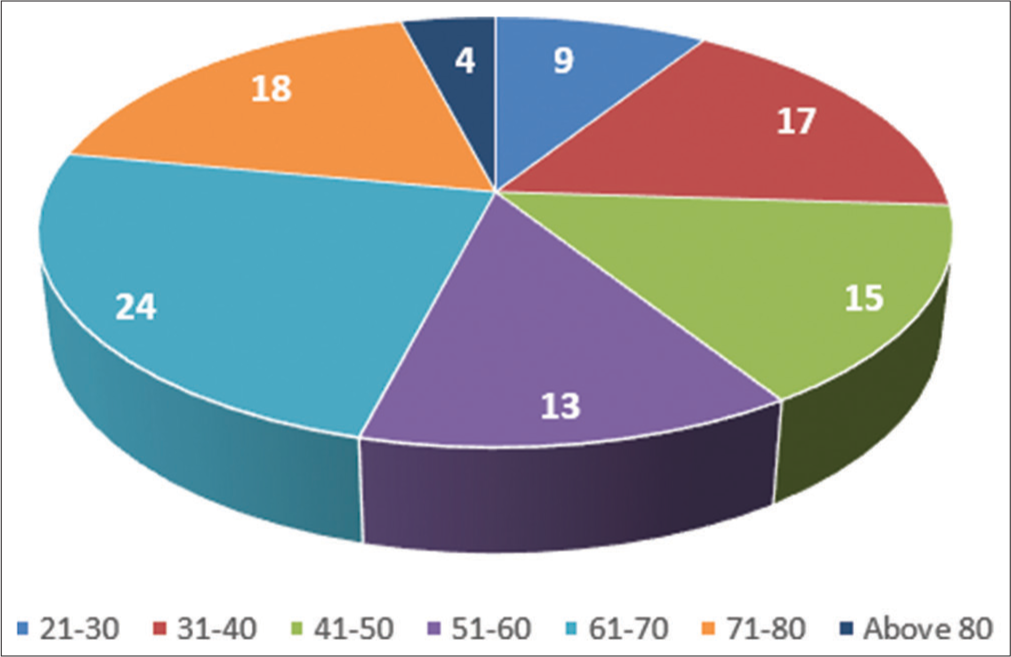
- Distribution of patients with respect to age group.
Figure 2: The most common occupation amongst the TB-tobacco patients were unskilled workers (34)..
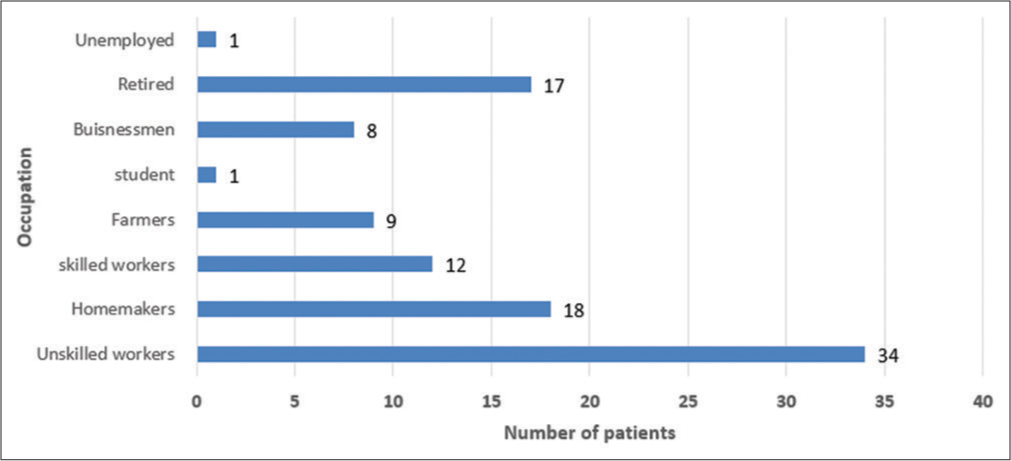
- Distribution of patients with respect to occupation.
Figure 3 shows that 39 TB-tobacco patients had only primary education and 37 had secondary education respectively.
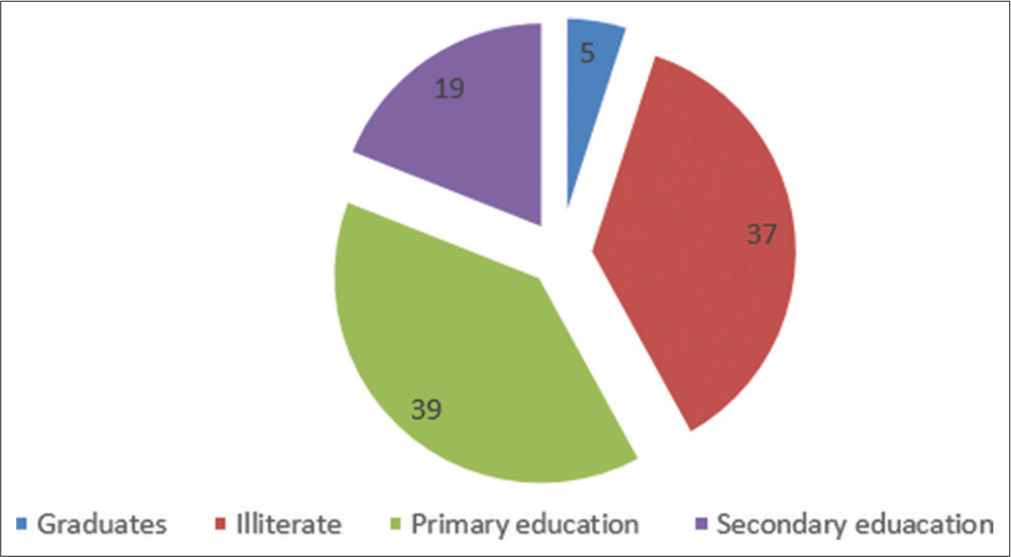
- Distribution of patients with respect to education.
Figure 4 shows that red/white patch was seen in 70 patients out of which 50 was seen on buccal mucosa of the oral cavity which was the most common site for (SLT) Smokeless tobacco in tuberculosis patients
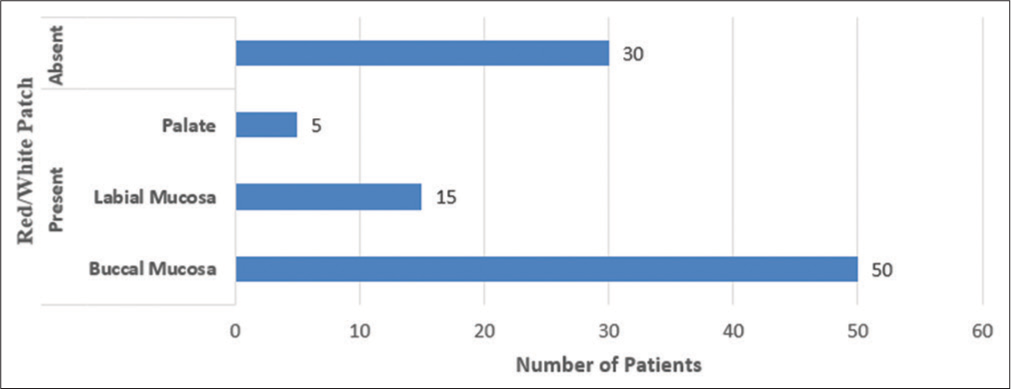
- Distribution of patients with respect to type and presence of oral mucosal lesion.
Figure 5 shows that 74 patients were consuming Smokeless Tobacco (SLT) amongst which 38 were chewing tobacco, 29 used tobacco mishri and 7 were consuming Gutka and 26 were consuming Smoked tobacco (ST) which included cigarettes (8) and Bidi (18).
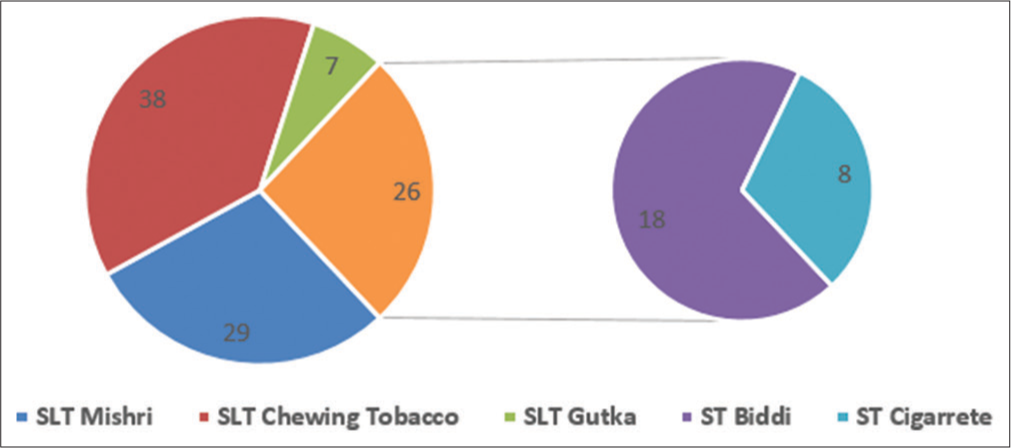
- Distribution of patients with respect to type of tobacco used.
Figure 6 shows that the most common factor responsible for the start of consuming tobacco was Peer pressure (35) followed by stress (31) in TB-tobacco patients.
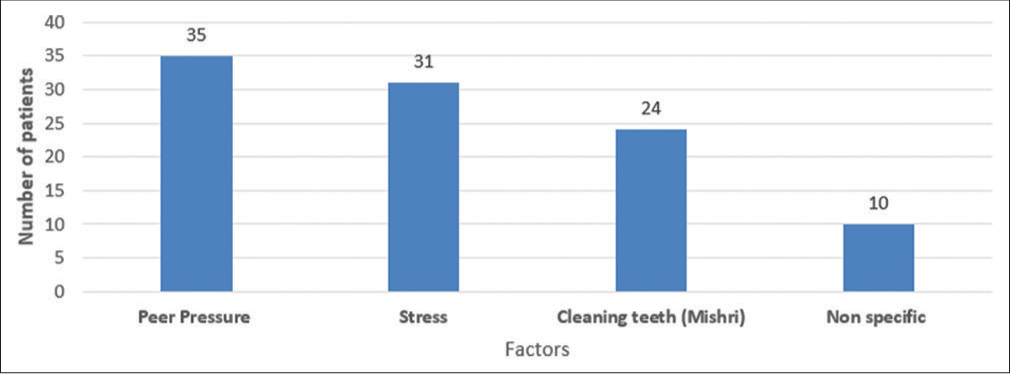
- Distribution of patients with respect to factors responsible for start of addiction.
Figure 7 The most common age at which tobacco use started amongst the TB-tobacco patients was 16-20 years (54)
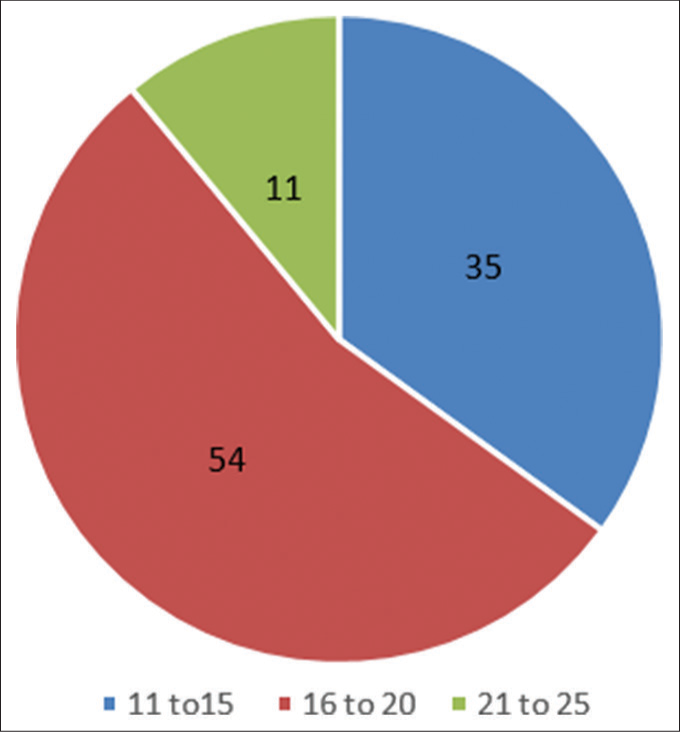
- Distribution of patients with respect to age of start of addiction.
Figure 8 shows that 36 of TB-tobacco patients were consuming tobacco in one or the other form more than 4 times a day.
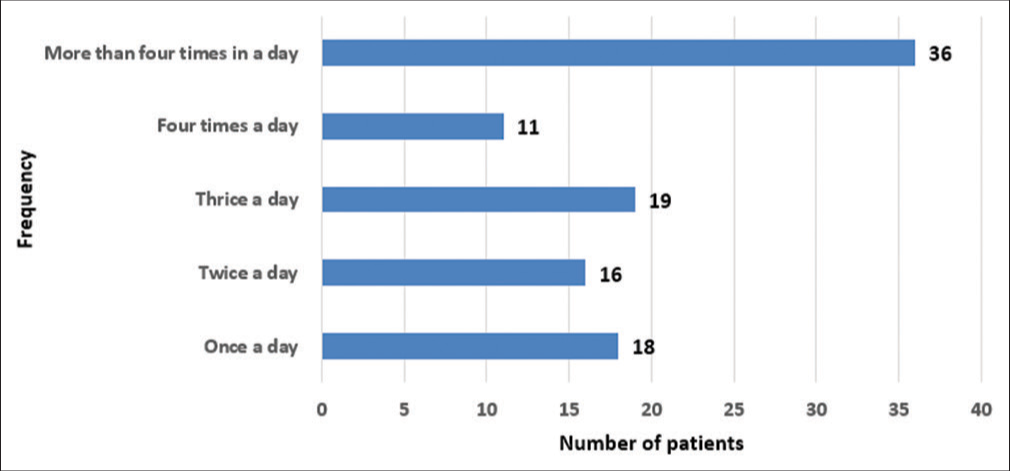
- Distribution of patients with respect to frequency of tobacco consumed per day.
DISCUSSION
One hundred patients diagnosed with TB on anti-tubercular therapy visiting the DOTS center between January 2022 and June 2022 consuming tobacco satisfying the inclusion and exclusion criteria were enrolled for the study.
Out of 100 TB-tobacco patients, the most common age group of TB-tobacco patients in the study was in between 61 and 70 years (n = 24) followed by 71 and 80 years (n = 18). This signifies that the elderly were the most common TB-tobacco patients [Figure 1]. The age findings are in contrast to the involvement of the younger population for tobacco use.[4,9] This may be due to only inclusion of TB patients who were using tobacco. Involvement of elderly tobacco users may also point toward increasing risk of occurrence of TB with the increase in duration of its use.[10]
In this study, we found out that 74 patients were male and only 26 patients were female in the study. Males were found to have a significantly higher percentage than females in the study may be due to the rural setup where males are more addicted to tobacco than females. Most common form of tobacco used by females was mishri. In India, adult males are expected to be more addicted than the females.[6,7,9] This gender difference in addiction behavior is reflected in our study.
The most common occupation among the tobacco addicted TB patients were unskilled workers (34%) [Figure 2] which are in accordance with the studies by Vellappally et al.[7] In our study, the unskilled laborers/workers were most commonly addicted to one or the other form of tobacco.
The results of our study show that 39% TB-tobacco patients had only primary education and 37% had secondary education, respectively, only 5% graduates were addicted [Figure 3] that this shows the trend that a higher percentage of people with higher education were less common among the study population. This is in accordance with the studies by Subramanian et al,[11] Vellappally et al.,[7] and Rani et al.[6]
On oral examination at baseline, red/white patch was seen in 70% patient out of which 50% was seen on buccal mucosa of the oral cavity which was the most common site for SLT in TB patients [Figure 4]. Oral mucosal lesions in the form of patches are due to continuous and frequent use of tobacco resulting in local irritation or chronic stimulation of lymphoid tissue in the oral mucosal membrane.[7]
In our study, we found that 74% patients were using SLT among which 38% were chewing tobacco, 29% used tobacco mishri, 7% were using gutka, and 26% were using smoked tobacco (ST), which included cigarettes (8%) and bidi (18%) [Figure 5]. Our results coincide with results of Vellappally et al.[7] In rural India, SLT use is higher than ST, chewing tobacco was the most common form of tobacco use. Mishri use was mostly recorded in rural female patients. Chaly found prevalence of bidis more than cigarettes, which are in accordance with our study (26% ST).[12]
On analysis of factors responsible for the use of tobacco among TB patient, we found that the most common factor responsible for the start of addiction was peer pressure (35%) followed by stress (31%) in TB-tobacco patients [Figure 6]. Our results are in accordance with studies of Nair et al.[13] Peer pressure is most commonly considered as one of the most important factors. In our study, the educational status and the age at which the addiction began reveals that the young primary or secondary school children are more involved may be due to peer pressure. The most common age at which tobacco use started among the TB-tobacco patients was 16–20 years (54%) [Figure 7].
In our study, 24% patients addicted to mishri were mostly unaware of the ill effects of tobacco and even about the content of tobacco in mishri. These females used mishri for cleaning teeth as a tradition which was seen in rural females more than the males. The findings of our study reveal that 36% of TB-tobacco patients were consuming tobacco in one or the other form more than 4 times a day, this percentage was lower than other studies.[14,15]
Overall, these studies highlight the high prevalence of tobacco use in India, with both smoking and SLT use being common among both males and females. The major reason would be occupational stress, as most of them were unskilled workers [Figure 8].
CONCLUSION
The present study contributed in assessing the oral health status and revealed that buccal mucosal patches were the most common patches seen in the oral cavity of tobacco addict’s TB patients. Among the patients using SLT, chewing tobacco, followed by use of mishri were most common forms of tobacco addiction. In tobacco addict’s TB, patients 16–20 years were the vulnerable age to start tobacco use, unskilled workers were the most common occupation among these patients.
Ethical approval
The research/study was approved by the Institutional Review Board at Pravara Institute of Medical Sciences-DU (UG/PG RMC), number PIMS/RMC/IEC-UG-PG/2002/127, dated 17th February 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Tobacco and tuberculosis: Could we improve tuberculosis outcomes by helping patients to stop smoking? Eur Respir J. 2015;45:583-5.
- [CrossRef] [PubMed] [Google Scholar]
- Global tuberculosis report 2014 In: Report No. WHO/HTM/TB/2014.08. Geneva: World Health Organization; 2014.
- [Google Scholar]
- Global TB report 2017. Available from: https://iris.who.int/bitstream/handle/10665/259366/9789241565516-eng.pdf?sequence=1 [Last accessed on 2022 Mar 14]
- [Google Scholar]
- Global adult tobacco survey: India 2016-17 report. Available from: https://ntcp.mohfw.gov.in/assets/document/surveys-reports-publications/global-adult-tobacco-survey-second-round-india-2016-2017.pdf [Last accessed on 2022 Apr 13]
- [Google Scholar]
- Tobacco in India. 2022. World Health Organization. Available from: https://www.who.int/india/healthtopics/tobacco [Last accessed on 2022 Apr 13]
- [Google Scholar]
- Tobacco use in India: Prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control. 2003;12:e4.
- [CrossRef] [PubMed] [Google Scholar]
- Tobacco habits and oral health status in selected Indian population. Cent Eur J Public Health. 2008;16:77-84.
- [CrossRef] [PubMed] [Google Scholar]
- Declaration of Helsinki- Ethical principles for medical research involving human subjects. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects [Last accessed on 2022 Apr 13]
- [Google Scholar]
- Tobacco use and nicotine dependence among newly diagnosed pulmonary tuberculosis patients in Ballabgarh tuberculosis unit, Haryana. J Family Med Prim Care. 2020;9:2860-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tobacco and tuberculosis: A qualitative systematic review and meta-analysis. Int J Tuberc Lung Dis. 2007;11:1049-61.
- [Google Scholar]
- Patterns and distribution of tobacco consumption in India: Cross sectional multilevel evidence from the 1998-9 national family health survey. BMJ. 2004;328:801-6.
- [CrossRef] [PubMed] [Google Scholar]
- Alert for an epidemic of oral cancer due to use of the betel quid substitutes gutkha and pan masala: A review of agents and causative mechanisms. Mutagenesis. 2004;19:251-62.
- [CrossRef] [PubMed] [Google Scholar]
- Tobacco use in India: A study of the prevalence and determinants of tobacco use among Indian adults. Indian J Public Health. 2017;61:48-53.
- [Google Scholar]
- Tobacco use among youth and adults in member countries of South-East Asia region: Review of findings from surveys under the Global Tobacco Surveillance System. Indian J Public Health. 2018;62:S17-23.
- [Google Scholar]







