Translate this page into:
Oral angioleiomyoma – A case report and its diagnostic challenges

*Corresponding author: C. S. Shobianand, BDS-Intern, Government Dental College and Hospital, Cuddalore, Annamalai Nagar, Chidambaram, Tamil Nadu, India. shobianand98@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shobianand C, Annamalai T, Shenbagaraj MP, Balasubramaniam V. Oral angioleiomyoma – A case report and its diagnostic challenges. J Academy Dent Educ. 2024;10:51-4. doi: 10.25259/JADE_101_2023
Abstract
A leiomyoma, an infrequently encountered entity in the oral cavity, is a benign tumor composed of smooth muscle. Its rarity in the head and neck region is attributed to the scarcity of smooth muscles. Typically located in the tongue, hard palate, or buccal mucosa, it manifests as a gradually enlarging submucosal mass. While it can develop at any age, it exhibits a higher incidence in females. This article aims to elucidate a case involving a 30-year-old female patient with a leiomyoma on the right buccal mucosa, providing detailed insights into clinical features, histopathological analysis, and the diagnostic challenges associated with this condition. The best line of treatment is surgical excision with a low recurrence rate and good prognosis.
Keywords
Benign smooth muscle tumor
Oral cavity
Leiomyoma
Angioleiomyoma
Spindle cell tumor
INTRODUCTION
Leiomyomas are typically found in anatomical sites abundant in smooth muscles. The scarcity in the head and neck region is explained by the fact that oral leiomyomas primarily originate from the middle layer of blood vessels, that is, tunica media, leading to their classification as vascular leiomyomas or angioleiomyomas. Even within the oral cavity, areas abundant in smooth muscles, such as blood vessels and salivary excretory ducts are most susceptible to leiomyomas. Oral angioleiomyomas have been observed in various oral locations, such as the palate, lips, tongue, buccal mucosa, and gingiva. The percentage of incidence in the female genital tract is 95%, skin is 3%, gastrointestinal tract is 1.5%, and infrequently over head and neck <1%.[1-3] In the oral cavity, its incidence is 0.065% due to the absence of smooth muscles. Its incidence among other soft-tissue tumor is only 0.42%.[4]
It is typically found in individuals aged between their fourth and fifth decades, with a predilection for females.[5,6] Leiomyomas usually present as a slow growing, small solitary nodule, round to oval in shape. Patients often present without any symptoms but are sometimes symptomatic with complaints of pain, mobile teeth, and mastication difficulty.
Types of leiomyomas according to the World Health Organization histological classification[7] are as follows:
solid leiomyoma
Epitheloid leiomyoma (leioblastoma)
Angiomyoma (vascular leiomyoma)
The incidence of epithelioid leiomyoma is 1%, solid leiomyoma is 25%, and angiomyoma is 74%.[8,9] The final diagnosis should rely on the histopathological examination and by immunohistochemical staining.
CASE REPORT
A female patient, 30 years of age, presented with the chief complaint of swelling in her right cheek region, persisting for the past 2 months. History of presenting illness revealed that the patient was apparently normal before 2 months later, she noticed a swelling in the left midface, which was asymptomatic. There was no history of associated illness and no relevant past medical, dental, and habit history.
Extraoral clinical examination revealed a swelling of size 3 × 3 cm evident in the right cheek region. It extended anteroposteriorly 1 cm from the corner of the mouth to 3 cm in front of the tragus of the right ear and super inferiorly 2 cm below the right zygoma to 3 cm above the right lower border of the mandible. Palpation revealed that the swelling was firm, and non-tender, with no bleeding or pus discharge.
Intraoral examination revealed an erythematous nodular submucosal mass of size 3 × 3 cm evident in the right buccal mucosa. It was located on the level of the occlusal plane. It extended anteriorly 1 cm from the corner of the mouth to posteriorly 0.5 cm in front of the right retromolar trigone. Superioinferiorly, it extended 1 cm from the upper buccal vestibule to 0.5 cm above the lower buccal vestibule. No surface ulceration was evident with well-defined margins. The surrounding mucosa appeared normal. Palpatory findings revealed a non-tender, fluctuant, and compressible mass [Figure 1].

- (a) and (b): Extraoral lesion site, (c): Intraoral lesion site, (d): Intraoperative image, (e): Biopsy specimen.
Following clinical examination, a provisional diagnosis of lipoma was arrived. Routine blood investigations were conducted. Subsequently, under local anesthesia, an excisional biopsy was performed and primary closure was executed. Then histopathological examination was done. After 1 week, the patient was recalled for review. The wound healing was satisfactory and suture removal was done.
Histopathological report
The hematoxylin and eosin (H and E)-stained sections of the soft-tissue specimen reveal connective tissue areas with intersecting/interlacing and swirls of spindle-shaped cells with diffusely interspersed vascular spaces of different sizes with extravasated Red blood cells (RBCs). The cytoplasm of the tumor cells is eosinophilic with nuclei appearing round-to-oval and elongated shape with tapered or blunt ends. The tumor cells seem to be surrounding blood vessels in most of the areas. Occasionally dispersed inflammatory cells, focal areas of tissue degeneration, and few adipocytes are also seen. In one section, muscle bundles are seen in close proximity to the tumor with an adjacent mass of adipose tissue. Since the tumor cells closely resemble vascular smooth muscle cells, sections were submitted to an immunohistochemical study.
Immunohistochemistry analysis
| Vimentin | Showed strong positivity in tumor cells |
| SMA | Showed diffuse strong positivity of tumor cell cytoplasm |
| CD 34 | Showed positivity in endothelial cells |
| Desmin | Showed focal positivity in tumor cells |
| S 100 | Negative |
| CD 68 | Negative |
SMA: Smooth muscle actin, S-100: Peripheral nerve sheath tumor marker, CD 34: Vascular endothelial progenitor cell marker, CD 68: Myeloid specific surface marker
The final histopathological report was suggestive of benign spindle cell neoplasm-angioleiomyoma.
DISCUSSION
The majority of oral tumors originate from the smooth muscle lining the walls of blood vessels, hence earning the designation of vascular leiomyomas or angioleiomyomas. It usually presents as a small tumor with an average size of 1–2 cm. The peak incidence is between 41 and 49 years, with a gender prevalence of females.[5,6] This case was a female patient with a lesion of size 3 × 3 cm and had a history of 2 months. Among the other histological variants of leiomyoma, the vascular leiomyoma incidence is high in the oral cavity due to the presence of increased blood vessels. However, the vascular variant of leiomyoma should be differentiated from hemangioma, pyogenic granuloma, and lymphangioma. All these are to be considered before arriving at the final diagnosis. Lesions with similar clinical presentation be considered are lipoma, neurofibroma, granular cell tumor, fibrous epithelial polyp, pleomorphic adenoma, hemangioma, fibroma, post traumatic fibroma, fibrous histiocytoma, and peripheral ossifying fibroma.[10] Histopathologically, one should consider the differential diagnoses such as benign spindle cell tumors such as schwannoma, neurofibroma, fibrous histiocytoma, nodular fasciitis, and malignant tumor such as leiomyosarcoma before arriving at the final diagnosis.[11-13]
Sharma et al., in 2018,[3] stated that differentiating leiomyoma from mesenchymal tumors with clinical features was quite difficult because they have a similar clinical appearance. The conclusive diagnosis of oral leiomyoma is predominantly determined through histopathological examination using hematoxylin and eosin stain. Using this stain we can differentiate leiomyoma that this stain show only minimal fibrous tissue compared to myofibromas.[14] This stain helps to differentiate the myofiborma with other smooth muscle lesion. Thus, in myofibromas, this staining shows much more collagenous stroma intermixed with the spindle cells, whereas in smooth muscle lesions, it will show only minimal delicate fibrous tissue surrounding the smooth muscle cells and in the septa between the smooth muscle masses.
In instances where H and E staining fails to provide adequate information, immunohistochemical studies can be conducted to reach a final diagnosis. Various smooth muscle markers such as desmin, muscle-specific actin, and smooth muscle actin (SMA) may exhibit positivity in smooth muscle tumors, while other markers such as S-100 protein, CD34 (transmembrane phosphoglycoprotein), cytokeratin, and epithelial membrane antigen can be employed for differentiation from other spindle cell tumors.
Distinguishing leiomyoma from a low-grade leiomyosarcoma can pose challenges. More than 10 mitotic figures in histopathological examination suggestive of malignant transformation [Figure 2].
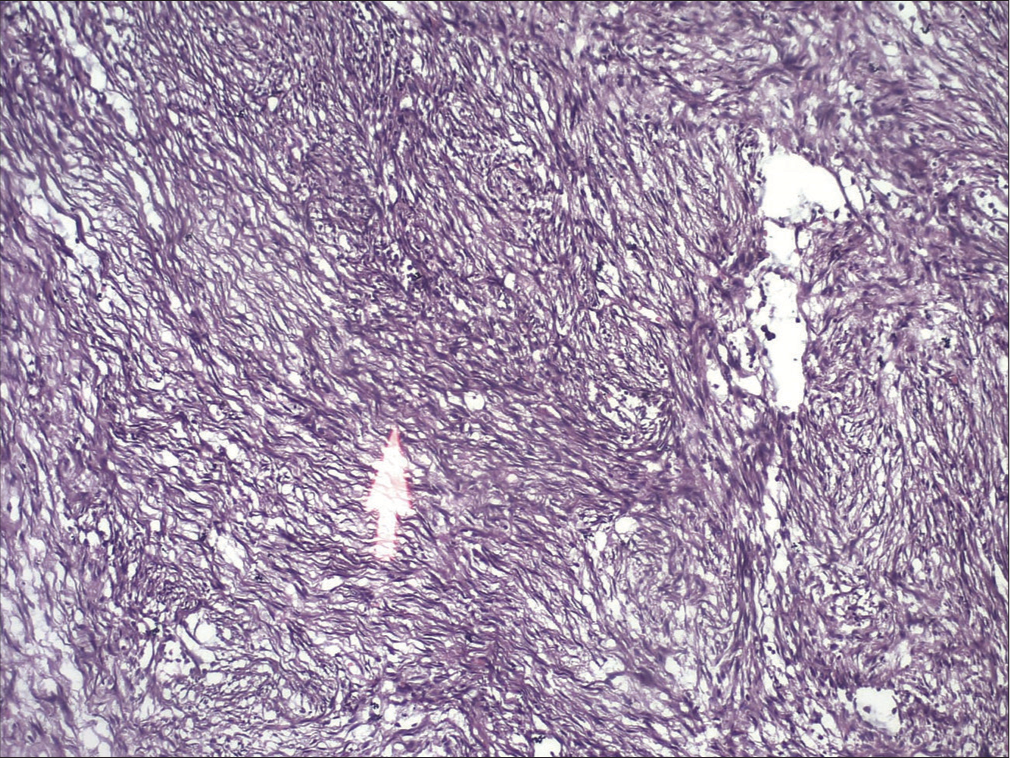
- Histopathological picture. (The white arrow signifies the connective tissue area showing interlacing swirls of spindle cells with extravasated Red blood cells).
The final diagnosis can be confirmed through immunohistochemical demonstration of actins. Actin, a small micro cytoplasmic filament with contractile properties, has six isotypes that differentiate between striated muscle, smooth muscle, and non-muscle cells. Anti-SMA exhibits good intensity and sensitivity for detecting leiomyoma.
Complete surgical excision is the primary and curative treatment for angioleiomyoma. Total excision of the mass was carried out, and recurrence is exceedingly rare.
CONCLUSION
Angioleiomyoma, a benign neoplasm composed of smooth muscle, seldom occurs in the oral cavity. It generally carries a favorable prognosis. Dental practitioners and oral pathologists should focus on the clinical context, possess a thorough knowledge of potential differential diagnoses, and conduct a meticulous evaluation of histopathological features. The judicious application of special stains and immunohistochemistry can assist in accurately interpreting the lesions.
The primary reliance for diagnosis lies in the histopathological analysis, and the utilization of stains such as SMA can be immensely beneficial. The preferred treatment is complete surgical excision with ample safety margins, resulting in a very low recurrence rate.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Nasal cavity vascular leiomyoma: Case report and literature review. Rev Bras Otorrinol. 2008;74:147-50.
- [CrossRef] [Google Scholar]
- Leiomyoma of oral cavity: Case report and literature review. Clin Exp Health Sci. 2017;7:81-4.
- [CrossRef] [Google Scholar]
- Oral leiomyoma: A case report on a rare lesion in oral cavity. J Oral Diagn. 2018;3:1-4.
- [CrossRef] [Google Scholar]
- Leiomyoma: A rare tumor in the head and neck and oral cavity: Report of 3 cases with review. J Oral Maxillofac Pathol. 2013;17:281-7.
- [CrossRef] [PubMed] [Google Scholar]
- Angioleiomyoma. A clinicopathologic reappraisal of 562 cases. Cancer. 1984;54:126-30.
- [CrossRef] [PubMed] [Google Scholar]
- Clinicopathologic characterization of oral angioleiomyomas. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2002;94:221-7.
- [CrossRef] [PubMed] [Google Scholar]
- Leiomyoma of oral cavity: Case report and literature review. Ann Stomatol (Roma)2011;. ;2:9-12.
- [Google Scholar]
- Oral leiomyoma: Report of a case. J Oral Maxillofac Surg. 1990;48:735-8.
- [CrossRef] [PubMed] [Google Scholar]
- Oral leiomyomas: Review of the literature and report of a case of palatal angioleiomyoma. J Periodontol. 1986;57:433-5.
- [CrossRef] [PubMed] [Google Scholar]
- Tumors of the oral cavity and pharynx. World J Surg. 2000;24:395-400.
- [CrossRef] [PubMed] [Google Scholar]
- Angioleiomyomas in the head and neck: A retrospective clinical and immunohistochemical analysis. Oncol Lett. 2014;8:241-7.
- [CrossRef] [PubMed] [Google Scholar]
- Vascular leiomyoma of the oral cavity. J Oral Maxillofac Surg. 1985;43:377-82.
- [CrossRef] [PubMed] [Google Scholar]
- Angioleiomyoma of the cheek: A case report. J Oral Sci. 2015;57:63-6.
- [CrossRef] [PubMed] [Google Scholar]
- Masson trichrome stain helps differentiate myofibroma from smooth muscle lesions in the head and neck region. J Formos Med Assoc. 2008;107:767-73.
- [CrossRef] [PubMed] [Google Scholar]






