Translate this page into:
Let the Light Heal - Lasers in Dentistry
*Author for correspondence
-
Received: ,
Accepted: ,
This article was originally published by Informatics Publishing and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Laser is one of the most captivating technologies in dental practice. Lasers in dentistry have revolutionized several areas of treatment in recent years. Introduced as an alternative to mechanical cutting device, laser has now become a most promising choice in many dental applications. Lasers evolved in dentistry have been widely used for various soft tissue and hard tissue applications. Various dental procedures like removing the caries, treatment of dental hypersensitivity, growth modulation, removal of calculus, recontouring and de-pigmentation of gingiva and other soft tissue procedures like frenectomy and gingivectomy etc. This article gives an insight into lasers in dentistry.
Keywords
Lasers
Photo Stimulation
Soft Tissue Lasers
1. Introduction
Periodontal therapy aims at removal of pathogenic biofilms, toxins and calculus, and creating a biologically acceptable root surface. The conventional periodontal therapy includes removal of calculus, treatment of food impaction, treatment of occlusal trauma and may also include pocket therapy and regenerative procedures. Patient discomfort in the above mentioned procedures also play a major role. Minimal tissue trauma, minimal patient discomfort and time are inevitable to achieve a successful periodontal management. Lasers can achieve excellent tissue ablation, strong bactericidal action and detoxification. It also improves healing1,2.
LASER is an acronym for ‘light amplification by the stimulated emission of radiation’.
2. Characteristics of Laser
Laser light is a single photon wavelength. When an atom is excited, it is stimulated to emit a photon by spontaneous emission. This causes release of subsequent photon. Laser light differs from ordinary light due to its properties like monochromatic, collimated and coherent. Laser has two wave forms. It can be continuous emission or pulsed beam emission. Pulsed beam is delivered as free running pulse or gated pulse. Laser light can be reflected, scattered, absorbed or transmitted to the surrounding tissues. Biological tissue contains free water molecules, proteins, pigments and macromolecules which is necessary for absorption1.
2.1 History of Lasers
The first laser was introduced during the 1917 by Albert Einstein which also lead to the invention of MASER (microwave Amplification by Stimulated Emission of Radiation). Gordon Gould introduced the acronym for laser in 1959. Theodore Maiman, in the 1960s, was the first to build a functioning laser in dentistry by using a mixture of helium and neon. In 1961 crystals of yttriumaluminium-garnet treated with 1-3 % neodymium was used to generate the laser. Argon laser was developed in 1962. In 1963 ruby laser was used to coagulate the retinal lesions. Carbon dioxide laser was developed in 1964. Diode lasers are being popularly used in dentistry.
2.2 Classification of Lasers
-
Soft tissue lasers
Diode laser
Carbon dioxide laser
Nd:YAG laser
-
Hard tissue lasers
Er:YAG laser
Er,Cr:YSGG laser
2.3 Based on the Type of Laser Material
-
Gas lasers:
Carbon dioxide laser, argonlaser, He-Ne laser
-
Liquid lasers:
Dye lasers
-
Solid state lasers:
Ruby lasers
Nd:YAG lasers
-
Semiconductor lasers:
Gallium, arsenide3
2.4 Laser-Tissue Interaction
When a laser beam hits the target tissue, it can have four basic interactions like reflection, scattering, absorption and transmission (Figure 1)4.
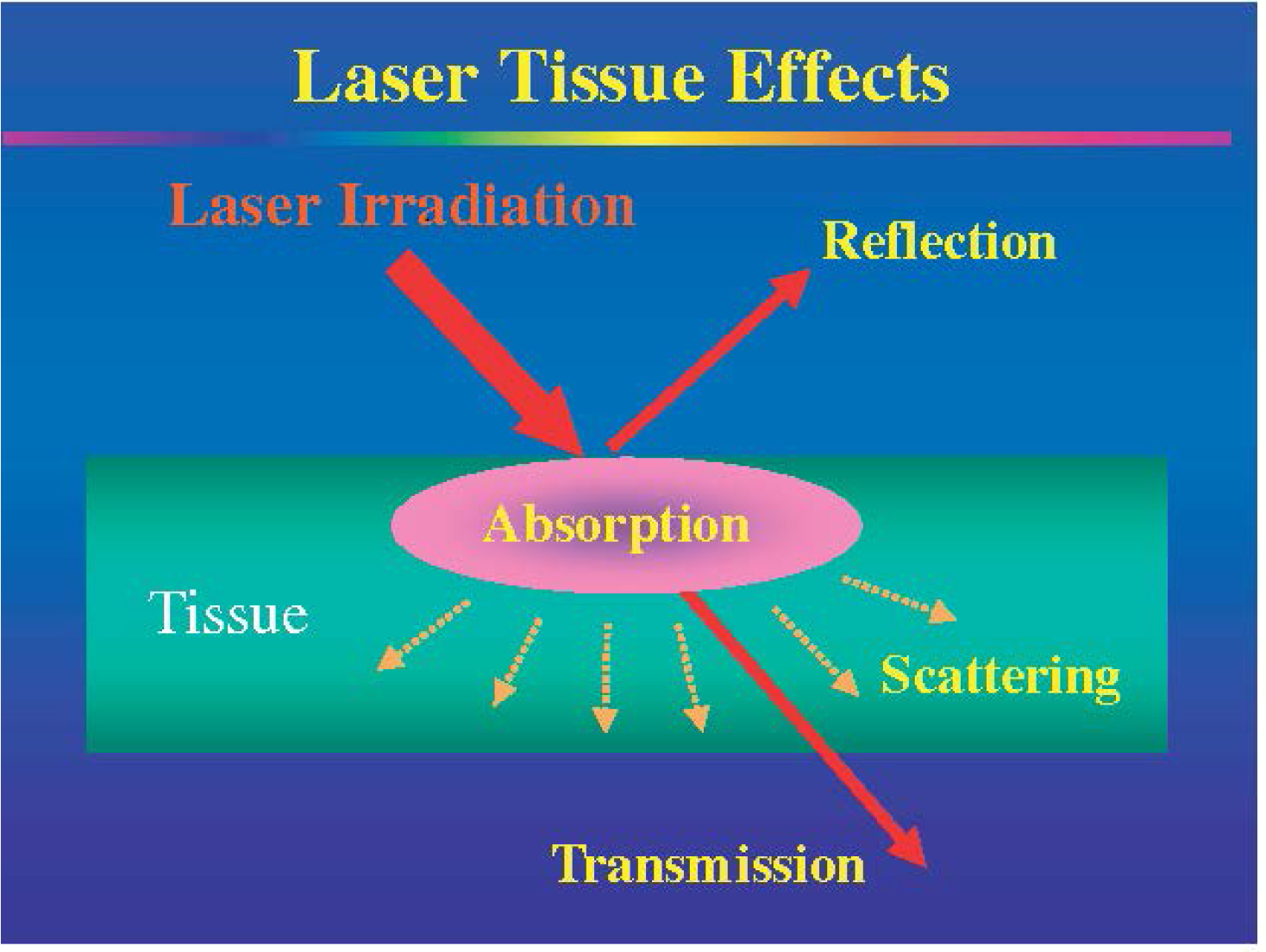
- Laser tissue effects.
Effects of laser on tissue include:
Photochemical-It has a stimulatory effect on biological tissues which induces healing and repair
Photothermal-The tissue is superheated and vaporized leading to coagulation and hemostasis.
Photomechanical-The laser light causes splitting up of the structures
Photoelectrical-In the high energy state, the semi gaseous particles form electrically charged ions and removes the tissue4.
3. Various Applications in Dentistry
Soft tissue procedures like incising, excising, coagulating, debriding the sulcus, gingivectomy, frenectomy, removal of mucocutaneous lesion and gingival sculpting techniques.
Hard tissue application includes removal of caries, cavity preparation, bleaching of tooth, removal of calculus.
Esthetic gingival procedures includes recontouring, reshaping of gingiva and crown lengthening procedures (Figure 3).
Laser is also used for the treatment of dentin hypersensitivity by occluding the dentinal tubules, de-epithelization, de-pigmentation (Figure 2), peri implant scar5.

- Laser depigmentation.

- Crown lengthening before Laser therapy.After Laser therapy.
4. Lasers in Operative Dentistry
Lasers can be used for cavity preparation using the intensive electromagnetic energy which ablates the tissue.
Erbium lasers are used due to its specific ablation. It also creates a microretentive pore which is used for composite restorations. Carbon dioxide laser has no thermal effects.
5. Lasers in Endodontics
The low intensity lasers have both analgesic and anti-inflammatory effect. This has got improved wound healing and reduced post-operative discomfort. The high intensity lasers like Nd:YAG and Er:YAG removes the bacteria in contaminated root canals
6. Lasers in Periodontics
The use of laser in periodontium is complicated because it contains both hard and soft tissues. Er:YAG, Nd:YAG and carbon dioxide lasers can be used to remove the hypoplastic gingival tissues. These procedures involve reduced scar formation and decreased post-operative pain. The Er:YAG laser has more antibacterial effect. With the use of laser, increased attachment level, reduced pocket depth and decreased plaque index are evident6.
6.1 Nd:YAG laser used for LANAP (Laser Assisted New Attachment Procedure)
Nd: YAG laser is used for removing the pocket epithelium, attaining hemostasis and removal of periodontal pathogens. Prior scaling is not necessary. Local anesthesia is given. The ‘first pass’ removes the lining of the periodontal pocket and also the periodontal pathogens8. Then, root debridement is done using piezoelectric ultrasonic tips. A blunt dissection is used to reflect the flap deep into the alveolar bone, thus changing the contour of the bone. Now, bleeding occurs which releases stem cells and growth factors. This is called ‘second pass’ where the blood is heated to obtain a thick fibrin clot. The flap is then attached to the tooth and bone. No sutures are required. Final occlusal adjustments are done7.
6.2 Lasers in Cosmetic Dentistry
Lasers are employed for tooth bleaching procedures without the use of chemicals. The argon and diode lasers are commonly used for office bleaching. Some lasers exhibit the properties of transmission and scattering which cannot be used due to its ability to penetrate into dentin and pulp6.
7. Conclusion
Dentistry has changed tremendously over the past decade to benefit both the clinician and the patient. Laser is one of the most captivating technologies which is being increasingly used in the field of dentistry. ‘Pain free’ and ‘simple procedures’ are the most attractive phases to those patients who are not willing to accept dental treatment. Thus, laser is a precise and effective way to perform dental procedures. Treatment with laser provides a hope of overcoming the disadvantages of conventional dental procedures.
References
- Lasers in nonsurgical periodontal therapy. Periodontology. 2000-2004;36:59-97.
- [CrossRef] [PubMed] [Google Scholar]
- Lasers in dentistry: An innovative tool in modern dental practice. Natl J Maxillofac Surg. 2012;3(2):124-132.
- [CrossRef] [PubMed] [Google Scholar]
- Lasers in minimally invasive periodontal and peri-implant therapy. Periodontology. 2000-2016;71:185-212.
- [CrossRef] [PubMed] [Google Scholar]
- Pulsed laser beam effects on gingival. J Clinic Periodontol. 1994;21:391-6.
- [CrossRef] [Google Scholar]






