Translate this page into:
CBCT – Cone Beam Computed Tomography
Address for Correspondence: Sahithya Kailash, Intern, Thai Moogambigai Dental College and Hospital, Chennai, India. E-mail: sahithyakailash@gmail.com
-
Received: ,
Accepted: ,
This article was originally published by Informatics Publishing and was migrated to Scientific Scholar after the change of Publisher.
How to cite this article: Kailash S. CBCT - Cone Beam Computed Tomography. J Dent Educ. 2014; 1(1):9–15.
Abstract
Dental X- Rays are important for diagnosing and treating patients by helping to detect oral health issues when they can’t be detected by visual or physical examination alone. Dental X-Ray take a much closer look and provide valuable information in the area of interest. Though 2 Dimensional X-Ray and Panoramic radiography can predict diagnosis in number of clinical cases, certain situations demand multiplanar imaging, one such technology is CBCT.
CBCT is a specialised 3Dimensional Craniofacial imaging in which 3 Dimensional reconstruction is possible. The final reconstructed image produced, reveals multilayer images in 3 orthogonal planes (coronal, sagittal and transverse)
This article focuses on CBCT and its applications in various fields of dentistry.
Keywords
Tomography
Radiation Dosage
Pathology Assessment
Treatment Planning
1. Introduction
CBCT was invented by Sir Godfrey N. Hounsefield in 1967. It was initially developed for angiography in 1982, subsequently applied to maxillofacial imaging. Only since late 1990s that it has been possible to produce clinical systems that is both inexpensive and small enough to be used in dental office.
Emergence of cone beam Computed Tomography has expanded the field of Oral and Maxillofacial Radiology.
A Brief History of CBCT (Siemens Medical Solutions, p. 1–35)
1885 Discovery of X- Ray radiation (Wilhelm Conroed Roentgen)
1896 First Chest X- Ray in Boston (F.H. Williams)
1903 Collimeter for suppressing scattered radia-tion was built (E.A.O Posche)
1913 High Vacuum hot – cathode was built (William D Collidge)
1930–1931 Planigraphy and stratigraphy was developed
1972 Development of Computed Tomography (Godfrey N. Housefield)
1974 First CT from a medical equipment manu-facturer.
1976 Whole Body CT
1978 ECG synchronised CT images
1989 First spiral CT
1992 Integrated CT angiography
1998 Cardio CT in routine operation
2002 16 slices per rotation
Recent advances: 64 slice CT, 4 Dimensional CBCT and Micro CT.
Synonyms
Dental Volumetric Tomography
Dental Computed Tomography
Cone Beam Tomography
Cone Beam
Preferred term is Cone Beam Computed Tomography It is a digital anolog of film Tomography
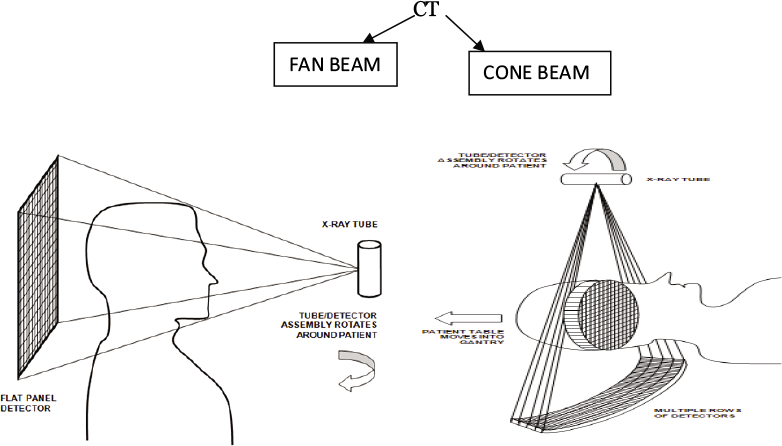
2. Computed Tomography
3. Principles of CBCT
CT scanner consists of X- Ray source detector mounted on a rotating gantry (Scrafe & Farman, 2006).
During rotation of gantry, the receptor detects X-Ray attenuated by patient.
These raw data are reconstructed by computer algorithm to generate cross sectional images.
-
CBCT is combination of
3Dimensional X-Ray beam
Circular collimation
Hence resultant beam is a cone beam. A single rotational scan of the gantry is necessary to acquire entire data required for reconstruction.
4. Radiation Dosage
CBCT unit results in higher radiation exposure than traditional dental radiograph; its radiation dose is lesser than that of medical Multichannel CT. Reducing the size of the irradiated area by collimation of the Primary X-Ray beam to the area of interest minimizes the radiation dose. Most CBCT units can be adjusted to scan small regions for specific diagnostic tasks. Radiation of a single CBCT scan is about 537 microsieverts (mean value) (Roberts, Drage & Dauies, 2009).
5. Patient Selection Criteria
In Accordance with the principle of ALARA, radiation dosage must be optimized. So that tissues of Clinical Interest receives radiation no greater than required for adequate imaging. CBCT should be preferred only when the potential clinical benefits will outweigh the risks associated with exposure to the ionizing radiation. Additional Consideration should be weighed prior to the exposure of children and adolescents.
CBCT should be considered adjunct to standard oral imaging modalities. Only if the conventional oral radiography does not determine the oral anatomy or further defined details needed, CBCT should be considered.
| Imaging Technique Effective Dose | Microseiver TS |
|---|---|
| Conventional Radiography | |
| Four-image posterior bitewings with photo-stimulable phosphor (PSP) or F-speed film and rectangular collimation | 5.0 |
| Panoramic radiograph with charge-coupled device | 3.0–24.3 |
| Cephalometric radiograph, posteroanterior or lateral with PSP | 5.1–5.6 |
| Full-mouth radiographs | |
| With PSP storage or F-speed film and rectangular collimation | 34.9 |
| With PSP or F-speed film and round collimation | 170.7 |
| CBCT | |
| Dentoalveolar CBCT (small and medium field of view [FOV]) | 11–674 (61) |
| Maxillofacial CBCT (large FOV) | 30–1073 (87) |
6. Strengths and Limitations
6.1 Strengths
6.1.1 Size and Cost
CBCT equipment has a greatly reduced size which can be easily accommodated in dental office. Cost is almost one fourth to one fifth to the Cost of CT.
6.1.2 High Speed Scanning
CBCT requires only single scan to capture necessary data compared with conventional CT scanners, hence scanning time is much reduced.
6.1.3 Image Accuracy-submillimeter Resolution
The Volumetric data set comprises a 3D block of cuboidal structures, known as voxels. The size of the voxels determines the resolution of the image. CBCT provides voxel resolution that are isotropic-equal in all three dimensions. This produces submillimeter resolution.
6.1.4 Low Patient Radiation Dose
As per International Committee on radiation protection, the effective dose for CBCT range from 52 to 1025 micro-sieverts (µSv) which 96%–51% less than of Conventional head CT(range 1400–21000 (µSv). Moreover, in CBCT X-ray beam can be collimated to reduce the irradiated area, thereby reducing the dosage and exposure. Patient radiation dose can be lowered by providing thyroid and cervical spine shielding.
6.1.5 Interactive Analysis
Acquired scan data are reconstructed through certain software which also provide extended applications for implant site assessment, Cephalometric analysis. Cursor driven measurements are also possible (White, & Pharoah, 2011).
6.2 Limitations
6.2.1 Image Noise
Image noise, a random variation of brightness or colour information in the images contributes to CBCT image degradation. Along with basic image protection certain other volume of radiation are irradiated, these are recorded as pixels on the cone beam area detector, It doesn’t actually reflect the object or anatomical site of interest (White, & Pharoah, 2011).
In homogeneity of X-ray Photon and increased X-ray beam divergence also causes image noise.
6.2.2 Poor Soft Tissue Contrast
X-ray photon intensities vary according to the tissue through which it is transmitted.
It differs with the density of the tissue, Anatomic number and thickness. There is scattering of X-ray Beam and that contribute to the poor soft tissue contrast (White, & Pharoah, 2011).
7. Applications
Implant site assessment
Endodontic application
Periodontal Application
Orthodontic Analysis
Cleft lip cleft palate assessment
TMJ assessment
Oral and Maxillofacial applications
8. Implant Site Assessment
Implant site assessment involves assessment of Bone density, quality and accurately depicting the vital structures in the area of interest. Though 2 dimensional panoramic and intra oral radiography are widely used in implant, its superimposed images hamper the detailed pre-operative planning of the implant procedures (American Dental Association council on scientific affairs, 2012).
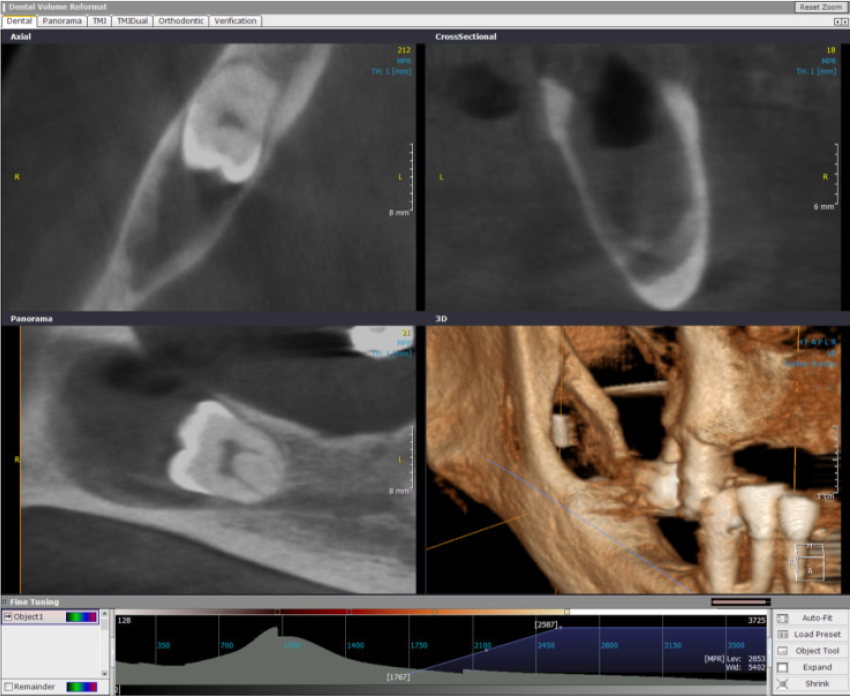
Selection of patient for implant placement is based on imaging of implant placement site. Bone density and thickness are most important factors that determine the success of the implant. Hounse field scale is used to measure radio density in reference to medical CT scan, can provide an accurate and absolute values which depict the bone density. CBCT are presented through gray values as well. Figure 1 shows axial and saggital sections showing buccal and lingual bone thickness and relationship between implant and inferior alveolar nerve.
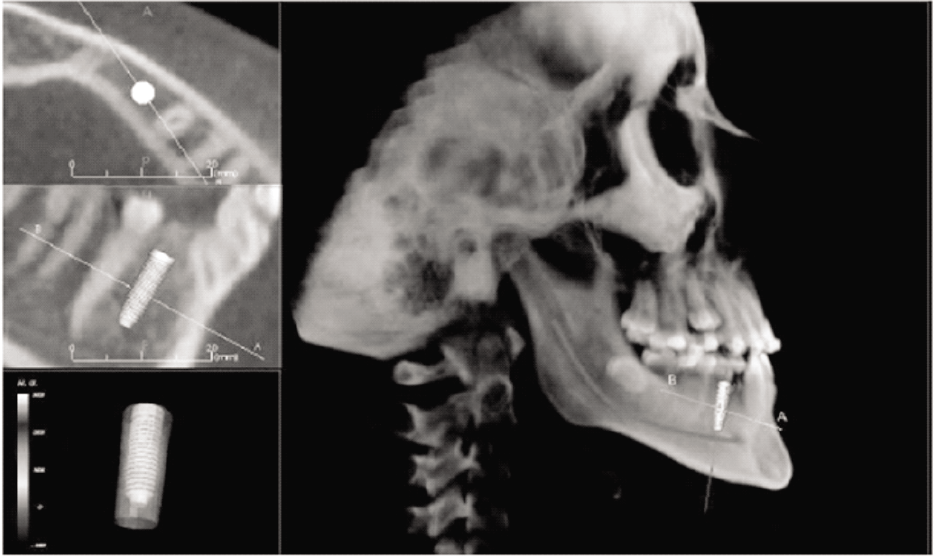
- Axial and sagittal sections showing buccal and lingual bone thickness and relationship between implant and inferior alveolar nerve. (Courtesy-3D Diagnostic Aid- CBCT in Orthodontics. Dr. SathyaChandran, Dr. Ramachandra Prabhakar, Dr. Saravanan et al. JOMIDA VOL-1 Issue-3-2013.)
The mean gray value (Mah, Reeves, & Mc David, 2010) for the four bone types:
TYPE I (dense)–362
TYPE II (porous cortical and course trabecular)–214
TYPE III (Porous cortical and fine trabecular)–76
TYPE IV (fine trabecular)–454
CBCT besides using as a diagnostic aid, it facilitates image guided surgery and virtual implant placement. A computerised tomographic scan derived surgical template is used for flapless surgery and immediate implant placement. Virtual implant placement allows us to plan surgery before the surgery is performed. There are softwares capable of emulating 3 dimensional surgeries in computer interface, decreasing the failure.
9. Endodontic Application
CBCT in Endodontics have aided in
Diagnosis of periapical lesions due to pulpal inflammation
Visualization of canals
Elucidation of internal and external resorption.
Detection of root fracture
Current 2D imaging is film based and digital based. Though Digital 2D imaging has improved diagnosis, certain limitations are unavoidable like in conventional radiographs periapical lesions are visible only if cortical plate is involved (Michetti, Maret, Mallet, & Diemer, 2010). Whereas, CBCT has enhanced visualization of lesions even before the lesion proceeds to produce radiological findings.
CBCT has proved useful for localization and characterization of root canals. It also helps to differentiate solid from fluid filled lesions (Periapical granuloma from cyst) using grey scale values in the lesions. These details would lead to more effective treatment of lesions. It also possible for more defined imaging of undisplaced root fracture, identifying the extent of internal resorption and localisation of a broken endodontic instrument.
CBCT is formed efficacious in endodontic surgeries and identification of dento alveolar trauma as well.
10. Periodontal Applications
More defined visualization of Lamina Dura, Crater defects, Furcation involvements and bone quality is possible through CBCT. CBCT images proved more potential in the morphologic description of periodontal bone defects. For Interproximal areas the visualisation through CBCT was as reliable as Periapical and bite wing radiographs (Tyndall, & Rathore, 2008). CBCT images were as same as that of clinical probing depth. In Buccal and lingual defects, CBCT was much superior to that of conventional radiography. CBCT may be a useful and more practical clinical tool than digital substraction radiography for the assessment of changes in periodontal bone overtime. When compared with conventional CT, CBCT has proved to be promising for periodontal applications, especially in the areas of intrabony defects, dehiscence and fenestration defects, periodontal cyst and in diagnosis of furcation involved molars.
11. Cleft Lip and Cleft Palate Assessment
Cleft Lip and Cleft palate being a congenital anomaly, radiological imagings are to be carried out in younger individual. Therefore attention must be paid to limiting the radiation exposure (Wörtche, Hassfeld, Lux, Müssig, Hensley, Krempien, & Hofele, 2006).
Considering the radiation safety in children, CBCT is used as 3 Dimensional imaging because of its low radiation exposure than 2 Dimensional CT. It immensely improves the diagnosis and pre-surgical plan as well.
12. Orthodontic Analysis
CBCT is used to determine (Chandran, Prabhakar, Saravanan, Karthikeyan, Vikram, & Prasath, 2013)
Facial growth
Airway function
Skeletal age
Disturbances in tooth eruption
3D Cleft tracing
Figure 4 shows lateral and antero posterior view enabling more precise cephalometric analysis and Figure 5 shows 3D cephalometric analysis.

- CBCT image showing root fracture and associated bone loss. (Courtesy: Oral Radiology- Principles of interpretation Stuart C White, Michael J. Pharoah).
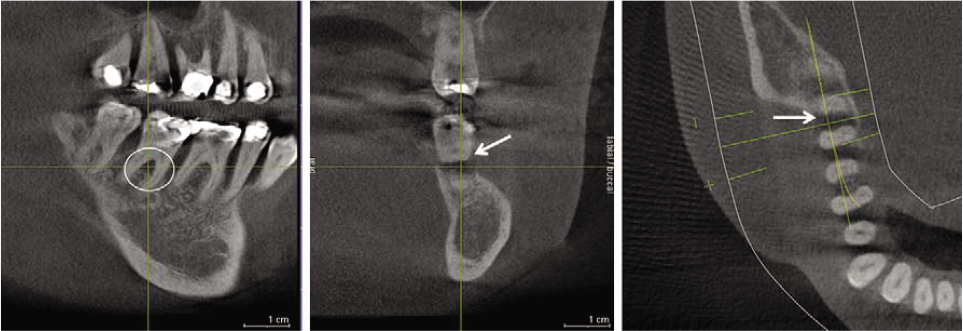
- Three images depecting a periodontal furcation involvement of a second molar (Picture Courtesy: Donald A. Tydall, Sonathe Rathore – The Dental science of North America).
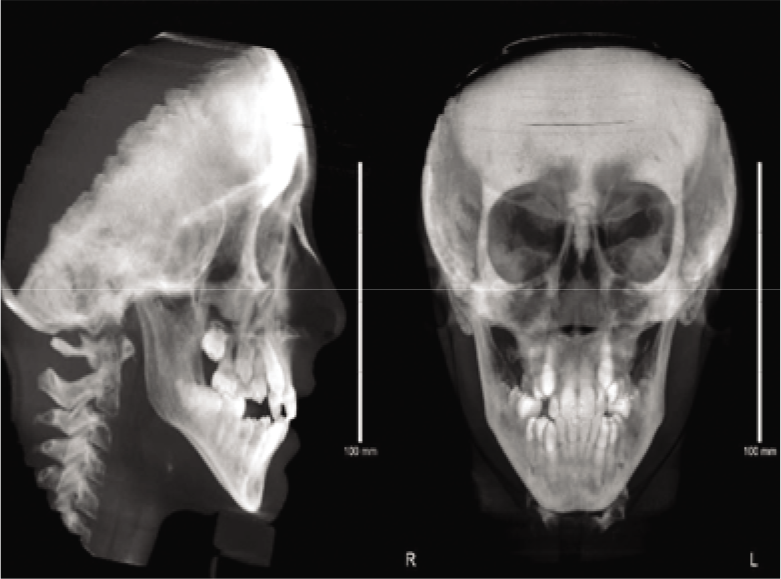
- Lateral and Anteroposterior View.
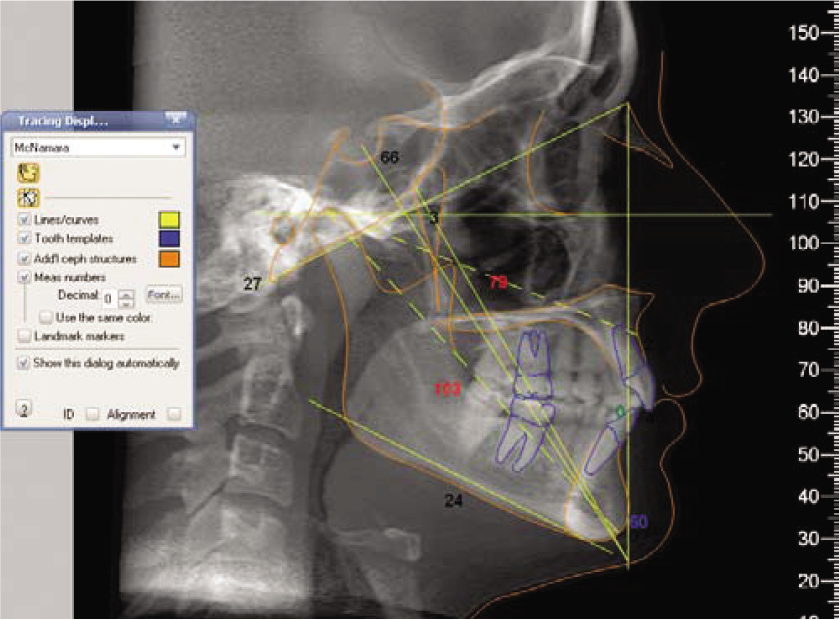
- 3D Cephalometric Analysis.
13. TMJ (Temporo Mandibular Joint)
TMJ imaging may be suggested in adjunct to clinical information in cases of osseous defects, worsening TMJ symptom, failure of conservative procedure, trauma, and significant dysfunction of joint, sensory and motor abnormalities. A number of imaging has developed over the years, but accurate imaging of all components of the complex anatomy of joint was not possible.
Recent Imaging modalities, like MRI and CBCT are now preferred for better understanding of pathologies of TMJ.
MRI is considered most useful diagnosis tool for TMJ as it provides images of both soft tissues and bony component, however it is contra indicated in few patients.
CBCT images can be produced in all 3 different planes hence all the components of the joint is simulated in reconstruction which gives real life image of the joint and the pathologies concerned (Tsikalkis, Syriopoulous, & Stamatakis, 2004).
Examining the joint with open mouth can be helpful in diagnosing internal derangement in the joint. Central and lateral views give information regarding the extent of translation of the condyle in the fossa. General view of open mouth gives clear view of condyle. Figure 6 shows CBCT image of Temporomandibular Joint pathology.

- CBCT image showing details of TMJ Pathology (severe arthritis with flattening of condyle). (Picture Courtesy: Radiographic Examination of temporomandibular joint using CBCT. K. Tsikalkis, K Syriopoulous and HC stamayakis).
14. CBCT in Oral and Maxillofacial Surgery
14.1 Tooth Impaction
Surgical removal of impacted teeth demands precise knowledge of the teeth location in the jaw and its relation to other anatomical structures. It is necessary to access the proximity of the impacted teeth to inferior alveolar canal in mandible, maxillary sinus in maxilla and palatal orientation of canine (Hassan, 2010).
Superimposition of adjacent structures impedes the assessment through 2 Dimensional radiographs. CBCT allows determining the exact location, orientation of the impacted tooth. Figure 7 shows close contact of nerve and impacted teeth in all dimensions.
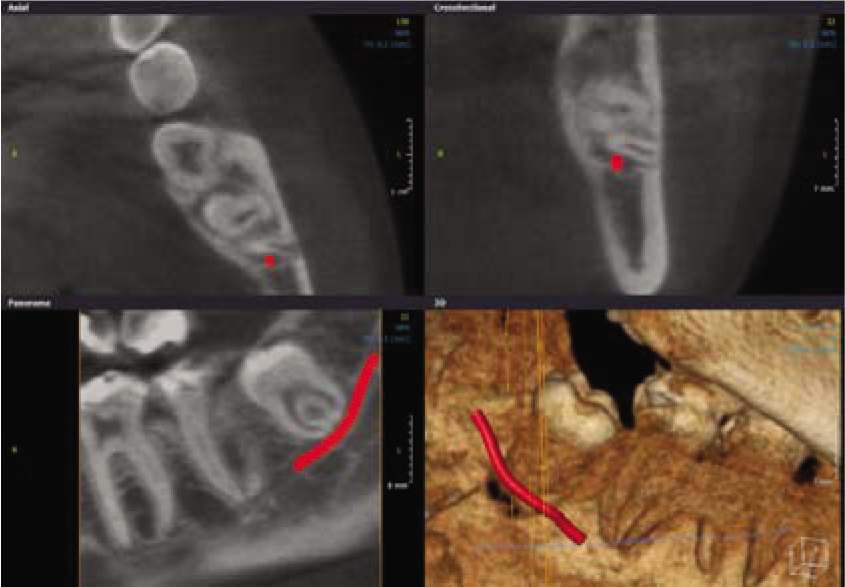
- Visualization of close contacts of mandibular canaland an impacted wisdom teeth. (Courtesy: Bassam Hassan. Applications of Cone Beam Computed Tomography in orthodontics and endodontic-ACTC Research Institute and the VU University of Amesterdam.
14.2 Pathological Conditions
CBCT are also used as diagnostic application in maxillofacial pathologies like osseous defects injuries, cyst lesions, calcifications of teeth and bone traumas and fractures. CBCT is also playing an increasingly important role in the detection of incidental pathology in patient referred to dental treatment. Unsuspected lesions in the para-nasal sinuses, parotid region are frequently detected. Figure 8 shows follicular dentigerous cyst with impacted teeth in right side of mandible.
- Folicular Dentigerous Cyst in the right mandible with an impacted tooth. (Picture Courtesy: R. Jacobs & P. Conto, Oral Imaging Centre, KU Leuven Belgium).
CBCT also plays a role in Radiotherapy for malignant tumors
It helps to reduce interfractional motion
Assess 3D status of tumour and helps in adaptive planning.
14.3 Orthognathic Surgery
Several applications of CBCT in orthognathic surgery treatment simulation, guidance and outcome assessment have been developed. Pre and Post operative CBCT skull models can also be superimposed to assess the amount and position of alterations in the mandibular ramii and condyle head following orthognathic surgery of maxilla and mandible.
15. Conclusion
CBCT is an emerging technology which has potential applications for imaging of high-contrast structures in the head and neck as well as oral and maxillofacial regions. It has undoubtedly increased dental practitioner access to 3Dimensional radiographic assessment widely in all fields of dentistry. One of the most clinically useful aspects of CBCT imaging is the highly sophisticated software that allows the huge volume of data collected to be broken, processed or reconstructed. Hence CBCT is a promising diagnostic aid in dentistry.
16. Acknowledgement
I would like to thank Dr. Rathika Rai, HOD, Dept of Prosthodontics and Dr. Ilango, Professor, Dept of Prosthodontics for their kind support and guidance.
Source of Support:
Nil,
Conflict of Interest:
None declared
References
- (2012). The use of cone beam CT in dentistry: an advisory statement. The Journal of the American Dental Association. ;143:899-902.
- [Google Scholar]
- (2013). 3 dimensional diagnostic aid-CBCT in Orthodontics. Journal of the Marthandom Indian Dental Association. ;1:28-31.
- [Google Scholar]
- (2010). Application of cone beam computed tomography in orthodontics and endodontics. ACTC Research Institute and the VU university of Amesterdam In: PhD Thesis.
- [Google Scholar]
- (2010)Deriving Hounsfield units using grey levels in cone beam computed tomography. Dento Maxillo Facial Radiology. ;39:323-335.
- [Google Scholar]
- (2010) Validation of CBCT as a tool to explore root canal anatomy. Journal of Endodontics. ;36:1187-1190.
- [Google Scholar]
- (2006) Clinical application of cone computed tomography in dental practice. Journal of the Canadian Dental Association. ;72:75-80.
- [Google Scholar]
- (2009) Effective dosage CBCT examination in dentistry. The British Journal of Radiology. ;82:35-40.
- [Google Scholar]
- (2004) Radiographic Examination of Temporomandibular joint using cone beam computed tomography. Dento Maxillo Facial Radiology. ;33:196-201.
- [Google Scholar]
- (2008). Cone Beam Computed Tomography Diagnostic Applications: Caries, Periodontal bone assessment and endodontic applications. Dental Clinics of North America. ;52:825-841.
- [Google Scholar]
- (2011). The book of Oral Radiology In: Principles and interpretation (6th ed). Elesevier, a division of Reed Elesevier India Private Limited;
- [Google Scholar]
- (2006) Clinical application of cone beam computed tomography in children with cleft lip & palate. Dento Maxillo Facial Radiology. ;35:88-94.
- [Google Scholar]






