Translate this page into:
Awareness of Potential Complications of Self-Medication- A “Selfie” Generation
*Address for correspondence:
This article was originally published by Informatics Publishing and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Self-medication is the major trend observed globally. Inadvertent consequences of self-medication include adverse drug reactions, incorrect dosage, and drug dependence to cite a few. A few of the common explanations fostering self-medication are formal education, family, availability of drugs and exposure to medical websites that provide information on diseases and health conditions. Patient prescriptions of friends and family are other sources utilized for obtaining over the table medicines. This short study is focused on the awareness of self-medication among patients and its potential adverse reactions.
Keywords
Adverse Drug Reactions
Self-Medication
1. Introduction
Self-medication is defined as “the use of drugs to treat self-diagnosed disorders or symptoms, or the intermittent or continued use of a prescribed drug for chronic/recurrent disease”1,2. In developing countries like India, self-medication is an important health concern with availability of over table drugs without a doctor’s prescription3,4. In some parts of India, patients adopt to self-medicate for minor symptoms due to shortage of human health care services in rural and tribal regions5. The major drawbacks of self-medication are delayed treatment, adverse drug reactions due to incorrect drug dosage, drug-drug interaction, incorrect route of administration and drug dependence6.
2. Aim
The aim of this survey is to study the awareness of self-medication and its potential complications among the patients.
3. Biomarkers
Two questionnaires with question relevant to self-medication and its consequences were given to participants of two study groups. The study groups were as follows
Group I- Patients with systemic disease.
Group II- Patients without systemic disease.
Each group comprises of fifteen patients above thirty years of age in each category mentioned above from both genders. Patients were given ten minutes answering the questionnaire (Figure 1, 2).

- Questionnaire for participants of Group I.
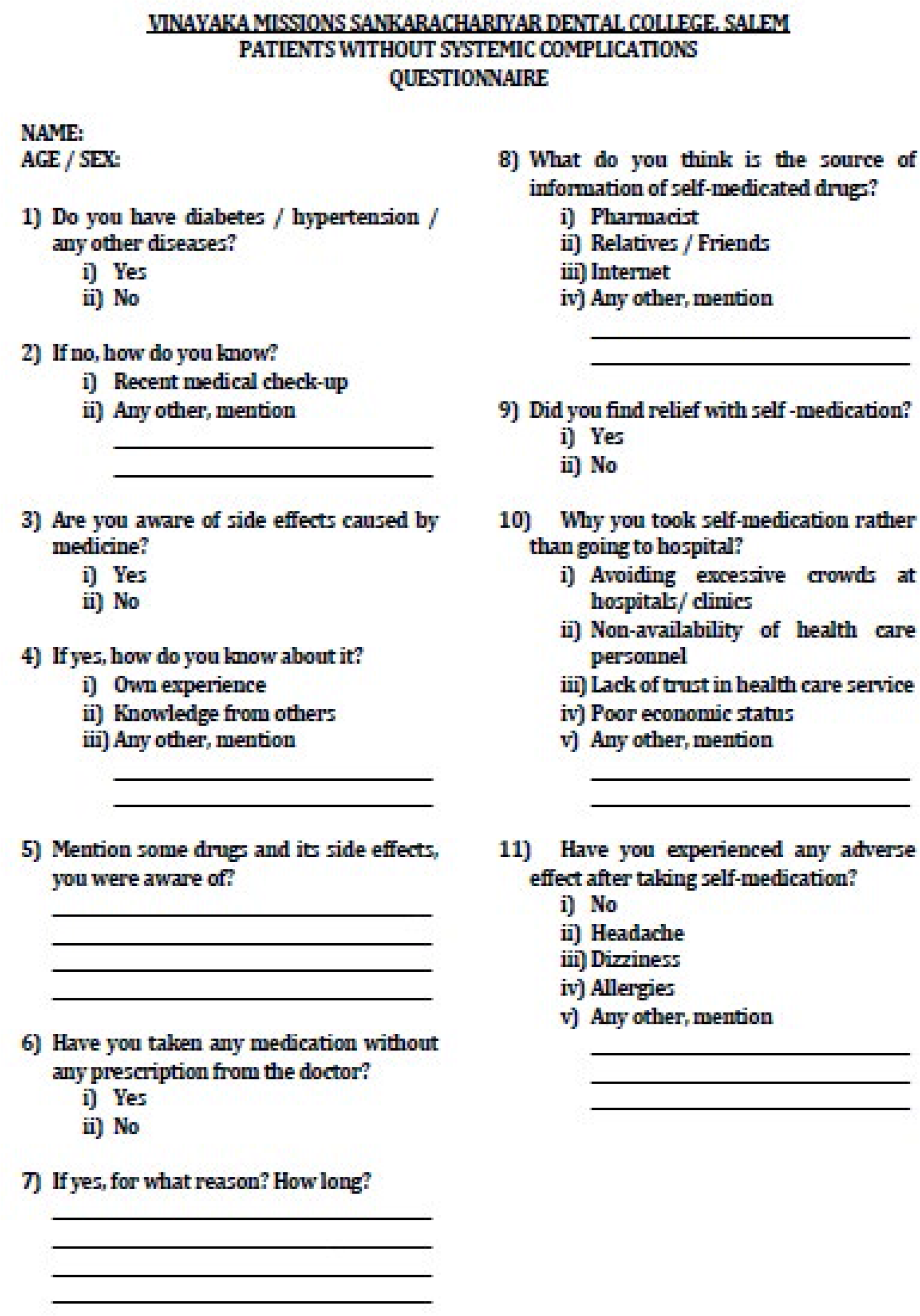
- Questionnaire for participants of Group II.
4. Results
The results are tabulated in Table 1 and the significant findings are as mentioned below.
About 18 of 30 participants are aware about the complications of self-medication i.e., 9 from each group, 7 males and 2 females in Group I and 2 males and 7 females in Group II.
There are 7 males and 2 females in Group I and 1 male and 7 females of Group II are aware of complications, yet resort to self-medication.
1 male from Group II is aware of complication and did not self-medicate.
2 males and 2 females of 30 participants who were affected by self-medication i.e., 2 from each group.
2 patients from Group I had experienced peptic ulcer and headache as side effects and 2 participants of Group II had vomiting and headache as side effects.
-
Even though, 9 participants of group 1 are aware about complication, the reasons behind self-medication were given as
-
Group I
To avoid excessive crowds in hospitals (2 males and 2 females).
Non-availability of health care nearby (1 female).
Poor economic status (3 males).
For minor illness (5 males).
To avoid injections (1 male).
For emergency (1 male).
-
Group II
To avoid excessive crowds in hospitals (1 male and 4 females).
Non-availability of health care nearby (2 males and 3 females).
Poor economic status (3 females).
The sources of self-medication were given as
Pharmacist - 6 males and 2 female.
Relatives/friends - 5 males and 1 female.
Other sources - 1 male.
-
| PARTICIPANTS | 30 participants | ||||
|---|---|---|---|---|---|
| GROUP I (15 participants) |
GROUP II (15 participants) |
||||
| S.No | MALE | FEMALE | MALE | FEMALE | |
| 1 | Number of participants | 12 | 3 | 4 | 11 |
| 2 | Patients with systemic diseases (i) Diabetic patients (ii) Hypertensive patients (iii) Asthmatic patients |
4 7 1 |
- 2 1 |
- - - |
- - - |
| 3 | Undergoing regular check-ups | 12 | 3 | 4 | 7 |
| 4 | Patients aware about the complications of self-medication | 7 | 2 | 2 | 7 |
| 5 | Patients aware about the complication, yet self-medicating | 7 | 2 | 1 | 7 |
| 6 | Patients aware about the complication, not yet self-medicated | - | - | 1 | - |
| 7 | Patients experienced side effects of self-medication (i) Peptic ulcer (ii) Headache (iii) Vomiting |
1 2 - |
- - - |
- - - |
1 - 1 |
| 8 | Reasons of self-medication (i) To avoid excessive crowd in hospitals (ii) Non-availability of health care nearby (iii) Poor economic status (iv) For minor illness (v) To avoid injection (vi) For emergency |
2 - 3 5 1 1 |
2 1 - - - - |
- 2 - - - - |
5 3 3 - - - |
| 9 | Sources of information (i) Pharmacist (ii) Relatives/Friends (iii) Internet (iv) Other sources |
6 5 - 1 |
2 1 - - |
2 - 1 - |
7 2 - 1 |
5. Discussion
In the present survey of thirty patients, almost sixty percent were aware of the complications of taking drugs with or without prescription. The fact remains that patients self-diagnose based on the proximity of symptoms to the particular organ and purchase drugs with reference to the symptom or prescriptions obtained from relatives or friends with similar symptoms. Furthermore, this practice is aggravated if the symptom for the underlying pathology is relieved by taking drugs obtained without proper medical advice. Around fifty percent of the patients in Group I were under medication for some systemic conditions and were aware of the complications of long term exposure to drugs thus preferred to visit a doctor for treating any ailment. The other fifty percent did take medications despite knowing the potential complications or adverse effects of taking medication with medical check-up.
The trend of self-diagnosis can be attributed to many reasons, primarily such as busy schedule, cost of visitations to a hospital and fear of being diagnosed underlying disease. The excuse of reduced health centres in rural areas and cost of drugs can be cited as reasons for the low income or socioeconomic classes. But the implicit nature of being knowledgeable of diseases and its treatment fosters patients to resort to self-medication. Almost fifty percent of the patients in this survey, were unaware of the inadvertent consequences to medications without doctor’s advice7,8.
Educating the general population by creating awareness of visiting a doctor for any symptom of disease in particular to infections can reduce the need for higher antibiotics due to rise in antibiotic resistance. Other complications as such as the effect long term use of NSAIDS on the kidney and liver.
Easy accessibility for health check-ups and affordability of drugs are initiatives that are to be adopted by both private and governments as well as in providing education, comprehensive health measures and a monitoring policy thereby reducing the prevalence of self medication.
6. Conclusion
From this short study, despite patients being aware about the complications of self-medication, they did resort to self-medication because of lack of health care personal nearby, to avoid excessive crowds in hospitals, poor economic status, and avoiding hospitals for minor illness. With rise in self-diagnosis and self-medication, educating the population on the potential adverse effects, complications and effects of long term use of drugs on internal organs is the need of the hour.
References
- Guidelines for the regulatory assessment of medicinal products for use in self-medication Geneva: World Health Organisation; 2000.
- [Google Scholar]
- Self-medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. Journal of Pharmacy and Pharmaceutical Sciences. 2005;8(2):326-331.
- [PubMed] [Google Scholar]
- Drug prescription and self-medication in India: An exploratory survey. Soc Sci Med. 1987;25:307-18.
- [Google Scholar]
- How and why are non-prescription analgesics used in Scotland? Fam Pract. 22:78-85.
- [PubMed] [Google Scholar]
- Common patient symptoms: Patterns of self-treatment and prevention. J Miss State Med Assoc. 1993;34:179-81.
- [PubMed] [Google Scholar]






