Translate this page into:
Assessment of awareness regarding rhinocerebral mucormycosis among undergraduate and postgraduate dental students: A cross-sectional survey

*Corresponding author: Nivedita Devalla, Department of Public Health Dentistry, Tamil Nadu Government Dental College and Hospital, Chennai, Tamil Nadu, India. nivedita.devalla412@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Devalla N, Selvamary AL, Kumar SGR, Anandhan S. Assessment of awareness regarding rhinocerebral mucormycosis among undergraduate and postgraduate dental students: A cross-sectional survey. J Academy Dent Educ. 2024;10:10-4. doi: 10.25259/JADE_32_2023
Abstract
Objectives:
The incidence of rhinocerebral mucormycosis (RCM), a fungal disease seen in immunocompromised individuals have drastically increased after the COVID-19 outbreak. The aim of the study was to assess the awareness of dental students regarding RCM.
Material and Methods:
An online cross-sectional survey was conducted among students pursuing BDS/MDS from various dental colleges in Tamil Nadu from August 2021 to October 2021. The questionnaire of 13 questions assessing awareness regarding RCM was administered using Google Forms. List-based random sampling method was used to sample the participants through e-mail and phone numbers of the students from college registries. Reminder calls were made every week to increase the response rate of the study. At the end of 2 months, the final data collected was organized using Google spreadsheets and subjected to statistical analysis through SPSS 22.0.
Results:
There were 597 respondents from 10 dental colleges, of which 172 were males, and 417 were females. Overall knowledge score for the disease ranged from 0.39 to 12.77 with a mean of 6.37. Postgraduates had greater knowledge in all categories of questions, except for causative micro-organisms, other forms of mucormycosis, its sources in the environment, and symptoms of RCM where there were no significant differences (P > 0.05) between preclinical, clinical undergraduates, and postgraduates.
Conclusion:
Awareness of dental students regarding RCM was found to be poor to average. Among the three study groups, postgraduates were most aware of the disease. Education and training programs on RCM are necessary for dental students to help them keep an eye out for features of rhinocerebral mucormycosis among the immunocompromised.
Keywords
Rhinocerebral mucormycosis
Coronavirus disease-2019
Survey
Dental students
INTRODUCTION
The year 2020 is a witness to one of the worst hit pandemics of humankind. The coronavirus disease-2019 (COVID-19) caused by SARS-CoV-2, not only inflicted sickness but also had far-reaching consequences on the future well-being after recovery from the disease, particularly among the immunocompromised.[1] It provided a safe haven for a wide range of opportunistic bacterial and fungal infections to grow and manifest as illnesses.[1] The prevalence of mucormycosis, a rare, fatal angio-invasive secondary fungal infection[2] commonly associated with COVID-19, was estimated to be around 140 per million in India[3] even before the pandemic, which is about 80 times higher than that of developed nations.[3] The incidence of COVID-19-associated mucormycosis has risen more rapidly during the second wave compared with the first wave of COVID-19 in India,[4] with more than 45,000 cases and about 4300 deaths during the second wave.[5]
Out of six clinical types of mucormycosis, the most common type and of great interest to the dentist is rhinocerebral mucormycosis (RCM).[2] It was found that nearly 79.4% of patients affected by mucormycosis were of rhinocerebral type,[1] of which 47.4% had involvement of maxillary sinus,[1] showing symptoms such as runny nose, low to high-grade fever, headache, blurred vision, unilateral or bilateral orofacial pain and swelling, loose teeth, periodontal tissue destruction, and appearance of black necrotic eschar in the palate, buccal vestibule, or the maxillary alveolus with the formation of oronasal/oroantral communication.[6] Since a bulk of manifestations is in the oral cavity, it becomes a golden area for early diagnosis of RCM. The disease is generally treated by early surgical debridement, rapid management of the underlying risk factor, and antifungal drugs, followed by reconstruction and rehabilitation after recovery.[6,7,8,9] Diagnosis of mucormycosis is often delayed, either due to clinical complications or due to misdiagnosis as symptoms of other diseases, especially COVID-19.[10] Despite advances in medical and surgical treatment options, the mortality rate among post-COVID-19 patients was found to be almost 50%.[9] Early diagnosis and intervention are the key to survival and prevention of morbidity in these patients.[8,9,10]
Health-care workers should be well equipped with the knowledge of clinical manifestations of the disease for prompt diagnosis and treatment. A study by Kabir et al. in 2021 revealed the mean knowledge score of health-care workers regarding RCM and its manifestations ranged from 21.89 to 29.55 over a maximum score of 30.[10]
Dental students are upcoming dental surgeons and it is expected that they stay updated on recent outbreaks of a disease and its manifestations, to impart quality treatment. Clinical undergraduate students, interns, and postgraduate students might come across clinical signs of mucormycosis among patients with dental complaints, during their posting in various departments. They should be confident in identifying, performing appropriate investigations, and thus diagnosing the disease early, enabling early intervention and improved chances for a better clinical outcome in these patients.
There is a paucity of research in the literature, assessing the awareness of dental students on RCM. This study is directed to evaluate the awareness of the disease among undergraduate and postgraduate dental students and to compare knowledge differences among pre-clinical undergraduate (1st and 2nd-year BDS), clinical undergraduate (3rd and 4th-year BDS and CRRI), and postgraduate (1st, 2nd, and 3rd-year) groups, if any.
MATERIAL AND METHODS
The awareness of RCM was assessed as a cross-sectional study done among dental students from various colleges in Tamil Nadu.
Ethics
Ethical clearance for the study is obtained from the institutional ethics and review board (5/IERB/2021) of the affiliated institution.
Study design
This is a cross-sectional survey.
Study population
The study population consists of students pursuing BDS or MDS.
Operational definitions
Pre-clinical undergraduate: BDS 1st and 2nd-year students
Clinical undergraduate: BDS 3rd and 4th-year students and CRRI
Postgraduate: MDS 1st, 2nd, and 3rd-year students.
Selection process
List-based sampling frame method – Random sampling method for online surveys.
Inclusion criteria
All undergraduate and postgraduate students from various dental colleges in Tamil Nadu were included in the study.
Exclusion criteria
Students whose contact details were found to be invalid.
Data collected
Demographic details
Self-assessed score for awareness of RCM in the range of 1–10
Thirteen questions assessing knowledge on RCM and one assessing attitude regarding early diagnosis
Self-assessed score for their confidence levels in diagnosis and treatment of RCM in the range of 1–10.
The present cross-sectional survey was conducted using an online survey form among the randomly selected students from the list of phone numbers of the dental students obtained from various college registries. Sixteen questions pertinent to the study were prepared after a thorough literature search in PubMed with keywords: Mucormycosis, RCM, COVID-19, oral manifestations, and management after applying relevant filters. The questionnaire was face and construct validated by a panel of experts and reliability was tested (Cronbach’s alpha 0.87). The pre-tested structured questionnaire consisting of sections on consent for participation, questions about sociodemographic details, knowledge, and awareness about RCM was made through Google Forms. The purpose of the study was informed to the students, and consent was obtained. The link for the survey was sent to the willing participants through phone numbers/e-mail. Reminder emails were sent to the non-respondents every week to improve the response rate for the study. The study was conducted for two months, and the students who had responded at the end of 2 months were taken as final respondents. The collected data were summarized by descriptive statistics, and the comparison of awareness between the pre-clinical, clinical undergraduate, and postgraduate students was done by Chi-square test using SPSS version 22.0.
RESULTS
From various dental colleges in Tamil Nadu, 1491 dental students (from 10 randomly selected dental colleges) were invited to participate, of which there were 597 respondents (response rate ∼ of 40%). There were 172 male participants and 417 female participants. Eight participants preferred not to reveal their gender. There were 253 pre-clinical undergraduates, 327 clinical undergraduates, and 17 postgraduates.
The majority of the students were aware of the causative microorganism (73%) and its sources in the environment (67.2%). Almost half of the participants were well informed on the mode of disease progression (42.2%) and frequent cause of mortality (55.8%). Only one-tenth of the students were completely knowledgeable about the population at risk (13.9%) and other forms of mucormycosis (9.5%). Almost the entirety of the students failed to identify all the given symptoms of RCM (correct = 0.3%). Most of them considered nasal stuffiness and headache as the only symptoms associated with the disease. Oral manifestations (3.9%), differential diagnosis (2.3%), investigations (4.9%), and treatment options (5.4%) were also minimally recognized. About one-quarter of the participants (24.8%) knew about the team of specialists involved, and only one-fifth (14.2%) wholly recognized the golden role of dentists, in diagnosis and treatment. About 86.4% of the survey participants agreed on the life-saving role of early diagnosis in the management of RCM [Table 1].
| S. No. | Question category | Percentage of correct answers | P-value* | |||
|---|---|---|---|---|---|---|
| Pre-clinical UGs | Clinical UGs | PGs | Total | |||
| 1. | Causative microorganism | 70.8 | 75.2 | 64.7 | 73 | 0.356 |
| 2. | Sources in the environment | 64.0 | 70.0 | 58.8 | 67.2 | 0.237 |
| 3. | Frequent cause of mortality | 50.6 | 59.0 | 70.6 | 55.8 | 0.059 |
| 4. | Population at risk | 10.3 | 15.9 | 29.4 | 13.9 | 0.001 |
| 5. | Mode of disease progression | 34.8 | 47.1 | 58.8 | 42.2 | 0.004 |
| 6. | Other forms of mucormycosis | 6.3 | 11.3 | 23.5 | 9.5 | 0.074 |
| 7. | Symptoms | 0 | 0.6 | 0 | 0.3 | 0.040 |
| 8. | Oral manifestations | 1.6 | 5.2 | 11.8 | 3.9 | 0.016 |
| 9. | Differential diagnosis | 1.2 | 2.8 | 11.8 | 2.3 | 0.001 |
| 10. | Investigations | 2.4 | 6.4 | 11.8 | 4.9 | 0.007 |
| 11. | Treatment options | 2.8 | 7.0 | 11.8 | 5.4 | 0.000 |
| 12. | Team of specialists | 17.8 | 29.7 | 35.3 | 24.8 | 0.001 |
| 13. | Role of dentists | 7.5 | 18.7 | 29.4 | 14.2 | 0.000 |
Knowledge score was computed, providing weightage for multiple-answer questions such as symptoms, oral manifestation, and differential diagnosis. Overall knowledge score for the disease ranged from 0.39 to 12.77 with a mean score of 6.37 ± 1.94. The mean self score for awareness and self-assessed level of confidence are found to be 5.10 and 5.17, respectively. No difference in awareness was noted between males and females.
A comparison of awareness was done between the pre-clinical, clinical undergraduate, and postgraduate students in overall knowledge score and self-assessed level of confidence [Charts 1 and 2].

- Overall knowledge score. UG: Undergraduate, PG: Postgraduate.
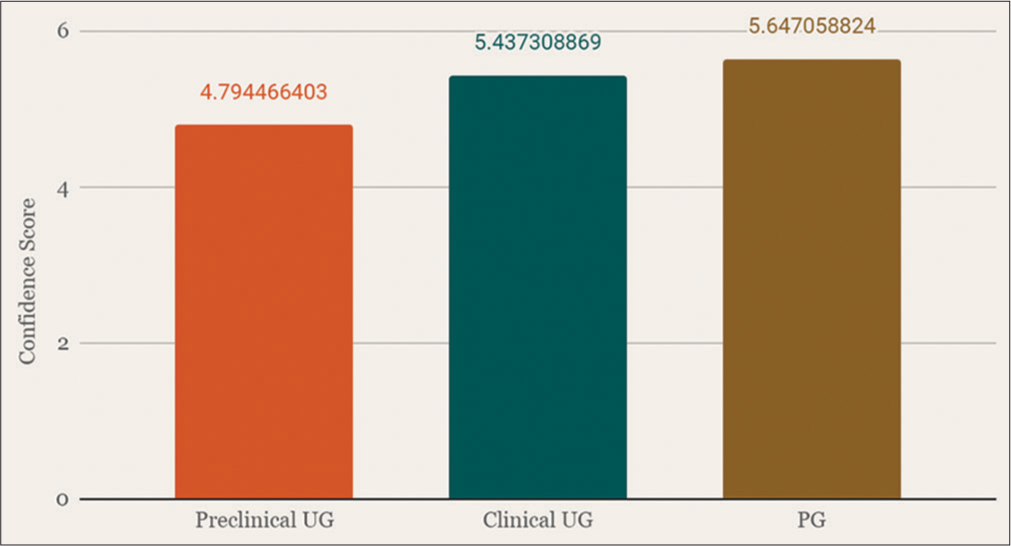
- Self-assessed level of confidence in diagnosis and management of rhinocerebral mucormycosis. UG: Undergraduate, PG: Postgraduate.
Performing inferential statistics using the Chi-square test, postgraduates were more aware of the disease, except for the other types of mucormycosis, causative micro-organisms, its sources in the environment, and symptoms, where there were no significant differences (P > 0.05).
DISCUSSION
India is deemed to be the “diabetes capital of the world,” home to nearly 28% of the urban population and 5% of the rural population affected by it.[11] India is also one of the countries worst affected by the COVID-19 pandemic, leading to a severe burden of mucormycosis (70%) among patients with diabetes mellitus and other conditions with compromised immune status.[11]
The online questionnaire in this study comprised various questions testing the knowledge of the disease, that is, the causative microorganism, its sources in the environment, the population at high risk for the disease, mode of disease progression, a frequent cause of mortality, other forms of mucormycosis, general signs and symptoms of the disease, oral manifestations, differential diagnosis, investigations, treatment options, the team of specialists involved in the treatment of the disease, and the role of dentists in diagnosis and management.
From the survey results, it is evident that the study participants were found to have poor to average knowledge of RCM. Their knowledge was found to be deficient in other forms, symptoms, oral manifestations, investigations, the team of specialists involved, and treatment options; the percentage of correct answers was found to be <10%. The students are often more confident in diagnosing commonly occurring diseases. There should be an incorporation of case reports and pictures concerning rare diseases and those associated with non-communicable diseases and immune deficiency diseases in textbooks for students.
Among the three study groups, postgraduates were most aware of the disease. They also perceived their knowledge to be high on RCM and were found to be more confident in diagnosing and managing the disease than pre-clinical and clinical undergraduates. This outcome may be due to their increased exposure to various clinical scenarios and evolution of knowledge, with years added in experience. However, they formed only 2.8% of the survey participants, which is a limitation of the study.
Most participants had a positive attitude toward the life-saving role of early diagnosis. There is a paucity of research studies assessing the awareness of RCM among dental students.
Patients with dental complaints may present with signs and symptoms of RCM. Clinical undergraduates and postgraduates manage most of the outpatients in dental colleges. Hence, they must know the disease to enable its identification in the early stages.
CONCLUSION
Studenthood is the most crucial period in the life of a health-care professional. It is during this time that their success as a good clinician is determined. Dental students, both undergraduate and postgraduate, must take an active part in learning about various diseases, especially those with their manifestations in the oral cavity. They should have an open and curious mind for learning and pursue to quench their thirst for knowledge. Education and training programs on RCM may be conducted for undergraduate and postgraduate dental students, to help them keep an eye out for features of RCM, especially among diabetic and other immunocompromised patients. They should emphasize and promote the importance of good oral hygiene practices, especially among the high-risk groups, to remove the oral nidus of infection and its consequences.
Acknowledgment
We acknowledge the Indian Association of Public Health Dentistry for providing us with a UG research grant to undertake this study.
Ethical approval
The authors declare that they have taken the Institutional Review Board approval and the approval number is 5/IERB/2021.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
The study was financially supported by a UG research grant awarded from the Indian Association of Public Health Dentistry.
References
- Mucormycosis in COVID-19: A systematic review of the literature. Infez Med. 2021;29:504-12.
- [CrossRef] [Google Scholar]
- Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15:102146.
- [CrossRef] [PubMed] [Google Scholar]
- Rising incidence of mucormycosis in patients with COVID-19: Another challenge for India amidst the second wave? Lancet Respir Med. 2021;9:e77.
- [CrossRef] [PubMed] [Google Scholar]
- Mucormycosis. Available from: https://www.who.int/india/emergencies/coronavirus-disease-(covid-19)/mucormycosis [Last accessed on 2022 Nov 25]
- [Google Scholar]
- Mucormycosis: India records more than 4,300 “black fungus” deaths. Available from: https://www.bbc.com/news/world-asia-india-57897682 [Last accessed on 2022 Nov 25]
- [Google Scholar]
- Dental and oral manifestations of COVID-19 related mucormycosis: Diagnoses, management strategies, and outcomes. J Fungi (Basel). 2021;8:44.
- [CrossRef] [PubMed] [Google Scholar]
- Risks of mucormycosis in the current Covid-19 pandemic: A clinical challenge in both immunocompromised and immunocompetent patients. Mol Biol Rep. 2022;49:4977-88.
- [CrossRef] [PubMed] [Google Scholar]
- Rhino-orbital-cerebral-mucormycosis in COVID-19: A systematic review. Indian J Pharmacol. 2021;53:317-27.
- [Google Scholar]
- World diabetes day 2018: Battling the emerging epidemic of diabetic retinopathy. Indian J Ophthalmol. 2018;66:1652-3.
- [CrossRef] [PubMed] [Google Scholar]
- Perception of mucormycosis infection among Bangladeshi healthcare workers: An exploratory cross-sectional study in the year following the COVID-19 pandemic. Bull Natl Res Cent. 2022;46:11.
- [CrossRef] [PubMed] [Google Scholar]
- Multicenter epidemiologic study of coronavirus disease-associated mucormycosis, India. Emerg Infect Dis. 2021;27:2349-59.
- [CrossRef] [PubMed] [Google Scholar]







