Translate this page into:
A minimally invasive approach on central giant cell granuloma: A case report

*Corresponding author: Keerthana Rao, Department of Oral and Maxillofacial Surgery, Sri Siddhartha Dental College, Tumkur, Karnataka, India. raokeerthy@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chandrodhayam V, Ashok Kumar KR, Rao K, Samantaray A. A minimally invasive approach on central giant cell granuloma: A case report. J Academy Dent Educ 2023;9:35-8.
Abstract
A rare, benign, and prying intrabony lesion that affects both the maxilla and the mandible, the central giant cell granuloma, is brought on by reactive or developmental defects. The most popular form of treatment is surgical curettage or, in cases of aggressive lesions, resection, but it is frequently impossible to avoid causing adverse impairment to the teeth or jaws, and recurrences seem more common. As a result, several subcutaneous administration methods using interferon alpha or calcitonin are documented in a number of case studies with varying degrees of efficacy. In this article, intra-lesional corticosteroid is used with no recurrence over a 2-year follow-up period to emphasize the value of a minimally invasive first line treatment.
Keywords
Cell granuloma
Intraosseous
Intralesional steroids
Triamcinolone
Non-surgical
INTRODUCTION
Central giant-cell granuloma (CGCG) is a rare, benign, and invasive intraosseous restricted lesion that affects the jawbones and accounts for 7% of all jaw cancers.[1]
The specifics of CGCG are unclear and debatable. Among the ideas put up are reactive lesions, developmental abnormalities, and benign neoplasms. Despite hypotheses that the lesion was caused by an aggressive inflammatory process or a neoplastic growth, the reason is still unknown.[2]
Neville et al. and the World Health Organization categorize it as a non-neoplastic lesion and designate it as a bone-related lesion despite the fact that this entity’s clinical behavior and radiographic findings typically mimic those of a benign tumor.[3,4]
In situations of aggressive lesions, surgical curettage demonstrated a high recurrence incidence; hence, resection with and without continuity faults was discovered to avoid relapse. There are many intralesional injections that can be used as a therapeutic approach, including steroids, calcitonin, interferon, bisphosphonates, and denosumab, to name a few. The goal of using medical alternatives or adjuncts to surgery in this young patient population was to avoid the need for resection and reconstruction.[5]
We present a case study of a multimodal treatment protocol used to treat an aggressive kind of CGCG. In this approach, the lesion was surgically curettaged after intralesional injections of corticosteroids.
CASE REPORT
A 25-year-old male patient came to our dental OPD complaining of pain and edema on the lower left side of his face for the past 5 months. When the patient’s history was obtained, it was discovered that he had the same nature of pain in January 2020 for which he visited a private clinic wherein he was given antibiotics and analgesics. Following which he noticed a swelling for which orthopantomogram (OPG) was advised and diagnosed as impacted 38. Surgical removal was attempted but stopped after mucoperiosteal reflection. A CT scan was advised and the patient was referred to our institute for further management in June 2020.
On extraoral examination, a large diffuse swelling with poorly defined margins was found on the left mandibular angle region, extending superoinferiorly from the midcheek region to the inferior border of the mandible and anteroposteriorly by 3 cm from the corner of the mouth to the tragus of the left ear [Figure 1]. Skin seemed normal above the swelling. Palpatory findings confirmed that the consistency of the swelling was hard and presented with mild tenderness. The lesion was non pulsatile, non-fluctuant, and non-reducible and was not fixed to the skin.

- Central giant-cell granuloma of the left mandible depicting a marked extraoral swelling and associated facial asymmetry.
An intraoral examination indicated obliteration of the buccal sulcus and swelling in the buccal vestibule extending from the distal aspect of the tooth 35 to the anterior border of the ramus [Figure 2]. Palpatory findings confirmed the swelling to be hard, tender, and non-mobile. Thirty-seven was tender on percussion. Vitality tests showed all the teeth to be vital.

- Obliteration of left lower buccal vestibule and pericoronitis of 38.
Aspiration of the lesion was done to rule out any cyst which was later found to be negative for aspiration. OPG reveals a radiolucent lesion associated laterally with impacted mandibular molar 38 extending up to mid ramal region [Figure 3].

- Orthopanthamogram depicting radiolucent lesion with associated impacted lower left third molar extending upto mid ramal region.
Computed tomography findings were suggestive of a well-defined multiloculated expansile lytic lesion measuring 4.4 × 3.2 × 2.9 cm in the left ramus of the mandible surrounding the roots of 3rd molar tooth [Figure 4].
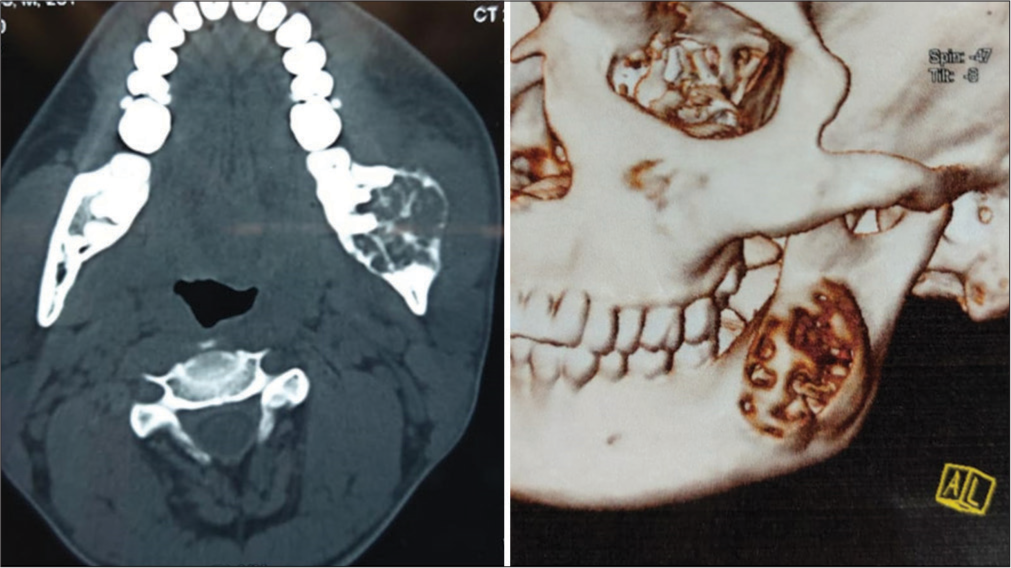
- Computed tomographic image depicting well defined multilocular expansile lytic lesion measuring 4.4 × 3.2 × 2.9 cm in left ramus of mandible with a 3D reconstruction.
An incisional biopsy was later planned and histopathological evaluation was done which revealed whorled collagen fibers and interspersed fibroblasts. The connective tissue stroma showed multinucleated giant cells with areas of hemorrhage and resorbing bone [Figure 5]. The reports were found to be consistent with CGCG.
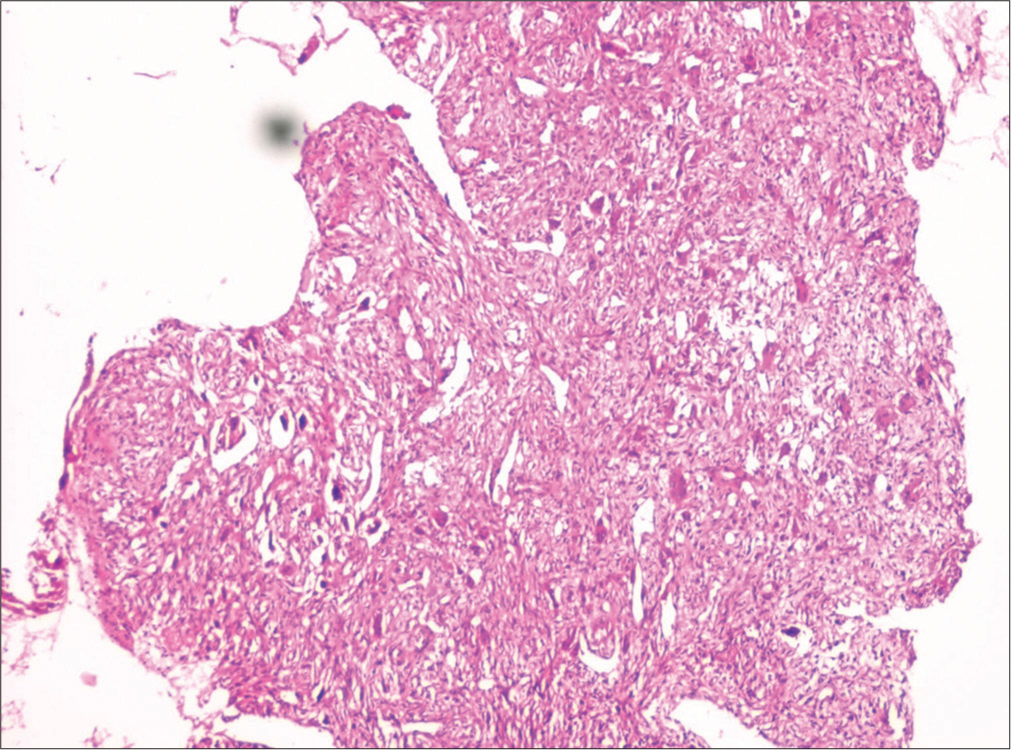
- Histopathological evaluation depicting whorls of collagen fibers and multinucleated giant cells suggestive of central giant cell granuloma.
The chosen treatment method in our situation was twice-weekly intralesional steroid injections for 3 months using 10 mg/mL triamcinolone (Kenacort-A) with 2% lidocaine [Figure 6]. The patient was monitored for the following 2 years, and there were no recurrences.

- Intralesional corticosteroid injection – 5 mL per injection of triamcinolone (10 mg/mL) with 2% lignocaine.
DISCUSSION
Jaffe claims that an intraosseous traumatic hemorrhage of the jaw can result in a CGCG, with young people and children being more prone to the lesion. These lesions typically appear before the age of 30, and more women than males are typically affected.[1]
In 1988, Terry and Jacoway were the first to describe treating a CGCG with corticosteroids. They recommended weekly intralesional injections of steroids to shrink the tumor based on its volume. Each cubic centimeter of the tumor will get 150 mg of prednisolone equivalent over the course of 6 weeks, according to the injection protocol. One patient in this study needed additional surgery, but three of the four patients made full recoveries.[6]
Due to the hypervascularization of the tumor, it is challenging to determine whether corticosteroids have a weak systemic dispersion due to intratumoral injection and the presence of epinephrine in the solution. After intralesional steroid therapy, one case of Cushing’s syndrome has been documented.[5]
The regressive response of CGCL to corticosteroid therapy may be brought on by the fact that multinucleated giant cells and mononucleated stromal cells in CGCL contain glucocorticoid receptors. The most popular drugs were triamcinolone acetonide (10 mg/mL or 40 mg/mL) and triamcinolone hexacetonide (20 mg/mL), all of which showed comparable efficacies. The injections were given once a week or twice a week. The most typical treatment plan involved six injections; however, cases involving up to 20 intralesional injections have also been documented.[7]
In line with the criteria established previously by Nogueira et al., 78.0% of CGCL patients responded favorably to intralesional corticosteroid injections, while only 7.3% had negative results. When only aggressive lesions were considered, 69.6% of cases demonstrated a favorable response to treatment, while 13.0% of cases demonstrated a poor response.[8]
Multinucleated giant cells that responded well to intralesional corticosteroid injections had increased glucocorticoid receptor expression, according to research by Nogueira et al. Although the majority of patients just received intralesional injections, further therapy may be necessary. In the present research, nine patients underwent aesthetic osteoplasty. Five instances had curettage, mostly to remove any leftover lesion tissue.[9]
Even though this procedure is less frequently performed and most patients opt for resection, it does seem to be more effective in treating unilocular tumors than multilocular tumors. This is likely due to the fact that a unilocular lesion is easier to access than a multilocular lesion, which can leave certain areas unscathed. It appears that this tactic works in about 50% of situations in the hands of those who employ it frequently, with a sizable failure rate.[10]
CONCLUSION
As a first-line therapy option for CGCG, intralesional corticosteroid injection may be offered. The lesion may completely disappear as a consequence of this treatment, or it may markedly shrink, enabling for a more prudent surgical strategy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Advantages and disadvantages of surgical and non-surgical treatment of central giant-cell granuloma: A review of literature. Int J Contemp Dent Med Rev. 2017;2017
- [Google Scholar]
- Total spontaneous regression of a central giant cell granuloma after incisional biopsy: A four-year follow-up case report. J Oral Maxillofac Surg. 2014;72:730-6.
- [CrossRef] [PubMed] [Google Scholar]
- Central giant cell lesion In: Barnes L, Eveson JW, Reichart P, Sidransky D, eds. World Health Organization Classification of Tumours Pathology and Genetics of Head and Neck Tumours. Lyon: IARC Press; 2005. p. :324.
- [Google Scholar]
- Injection of steroids intralesional in central giant cell granuloma cases (giant cell tumor): Is it free of systemic complications or not? A case report. Int J Surg Case Rep. 2015;8C:166-70.
- [CrossRef] [PubMed] [Google Scholar]
- Management of central giant cell lesions-an alternative to surgical therapy. Oral Maxillofac Surg Clin North Am. 1994;6:579-600.
- [CrossRef] [Google Scholar]
- Intralesional corticosteroid injections in the treatment of central giant cell lesions of the jaws: A meta-analytic study. Med Oral Patol Oral Cir Bucal. 2013;18:e226-32.
- [CrossRef] [PubMed] [Google Scholar]
- Intralesional injection of triamcinolone hexacetonide as an alternative treatment for central giant-cell granuloma in 21 cases. Int J Oral Maxillofac Surg. 2010;39:1204-10.
- [CrossRef] [PubMed] [Google Scholar]
- Glucocorticoid and calcitonin receptor expression in central giant cell lesions: Implications for therapy. Int J Oral Maxillofac Surg. 2012;41:994-1000.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and management of giant cell lesions of the jaws. Ann Maxillofac Surg. 2012;2:102-6.
- [CrossRef] [PubMed] [Google Scholar]






