Translate this page into:
Recent trends in dental ceramics: A comprehensive review

*Corresponding author: Akash Raj Sharma, Department of Prosthodontics and Crown and Bridge, Subharti Dental College and Hospital, Meerut, Uttar Pradesh, India. itsdocakash@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma R, Sharma AR, Madathil E, Tayal R. Recent trends in dental ceramics: A comprehensive review. J Academy Dent Educ. 2025;11:61-7. doi: 10.25259/JADE_37_2024
Abstract
Ceramics have proven to be highly versatile materials that serve various purposes in everyday life. Their introduction into dentistry has led to their utilization in numerous forms, starting with the commonly known term porcelain. Over time, ceramics in dentistry have evolved to a new standard, offering a wide range of applications from simple inlay restorations to full-mouth rehabilitation. With technological advancements such as computer-aided design/computer-aided manufacturing and 3D printing, ceramics are becoming increasingly popular in dentistry. They are not only used as graft materials but also in implantology due to their high biocompatibility. This literature aims to highlight the modifications that have taken place in the field of dentistry concerning ceramics.
Keywords
Ceramics
Composite
Computer-aided design/Computer-aided manufacturing
Esthetics
Implants
INTRODUCTION
In the modern era, individuals are focused on enhancing their self-esteem. It is widely recognized that a beautiful smile, which looks natural, can significantly boost one’s self-confidence. As a result, esthetics have become a key factor in a patient’s decision to visit a dentist. Patients now expect their treatment to result in a smile that is visually pleasing. Dental ceramics have played a crucial role in helping dentists meet the growing demand for esthetics.
Ceramics have emerged as a popular choice in dentistry due to their ability to closely mimic the appearance of natural tooth structure. These materials have effectively addressed the issue of compromised esthetics often associated with traditional all-metal restorations while maintaining the strength and durability of the final restoration.[1]
To meet the increasing esthetic demands, alternative restorative materials such as composites, polymers, and others have been extensively studied. Numerous research studies comparing the physical properties and biocompatibility of these materials with dental ceramics have consistently shown that ceramic materials possess superior strength, hardness, elastic modulus, and a more biocompatible nature. These findings explain the widespread use of ceramic materials in the field of dentistry [Figure 1].[1,2]
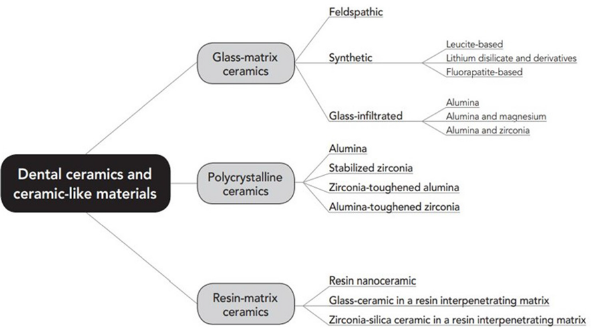
- Overview of the proposed classification system of all-ceramic and ceramic-like materials.
Traditional feldspathic ceramics, which consist of Feldspar, Quartz, Kaolin, and other substances, had the drawback of being brittle and causing wear on natural teeth that oppose them. To overcome this limitation, advancements have been made in the development of ceramic materials by altering the microstructure or processing methods of conventional ceramics.
The objective of this article is to provide a comprehensive overview of the latest advancements in ceramic dentistry, including a discussion on CAD/CAM technology and the introduction of 3D printing for dental ceramic restorations. This knowledge will empower clinicians to select the most suitable ceramic material for specific clinical scenarios.
DISCUSSION
Advances in microstructures
The fundamental structure of any material is determined by its microstructure. To bring about a change in the material’s clinical properties, it is necessary to modify its microstructure.
For a long time, ceramics have been categorized based on their microstructure. One commonly used classification system, developed by Kelly and Benetti,[2] categorizes ceramic materials according to their glass content. This system can be described as follows: (1) Materials that are predominantly glassy, (2) glasses filled with particles, and (3) polycrystalline ceramics that do not contain any glass.
However, this classification system, along with several others, does not consider resin-matrix materials that are heavily filled with ceramics. These materials have recently been designated as “Ceramic Material” by the American Dental Association. In light of this, a new classification system for ceramic materials has been proposed by Gracis et al.[3]
Glass-matrix ceramics: non-metallic inorganic ceramic materials that contain a glass phase.
Polycrystalline ceramics: non-metallic inorganic ceramic materials that do not contain any glass phase.
Resin-matrix ceramics: polymer matrices that predominantly consist of inorganic refractory compounds, which may include porcelains, glasses, ceramics, and glass ceramics.
Glass-matrix ceramics
Feldspathic: Glass-matrix ceramics belonging to the traditional group are based on a ternary material system consisting of clay/kaolin, quartz, and naturally occurring feldspar. These ceramics are known for their high brittleness, limiting their use as veneering material on metal alloys and ceramic substrates. Examples include IPS Empress Esthetic, IPS Classic, Vita VMK 68, and Vitablocks.[4]
Leucite-reinforced glass ceramics: This type of synthetic ceramic material is made up of Potassium Aluminum Silicate dispersed in a glass matrix and baked at 1020°C. It exhibits good translucency and increased resistance to crack propagation due to the crack deflection property of leucite crystals. These ceramics offer good esthetics but reduced strength, making them suitable for use in low-stress bearing areas such as Anterior crowns, Inlay, and Onlay. Examples include IPS Empress, among others.
Fluorapatite-based glass ceramics: Fluorapatite-based glass ceramics exhibit a phase of fluorapatite crystals during processing, providing them with good modeling properties, high strength, and excellent firing behavior. They are recommended for use as materials for characterization and veneering of conventional Lithium Disilicate and Zirconium oxide glass ceramics. An example is IPS e-max Ceram, a nano fluorapatite glass ceramic.[5]
Lithium disilicate reinforced glass ceramics: Among the earliest synthetic glass matrix ceramics, these ceramics are composed of 70% lithium disilicate crystals. They offer excellent esthetics, chemical durability, and stability, along with high strength due to the interlocking nature of leucite crystals with the glass crystals. These properties make them ideal for use as Veneers, Anterior/Posterior crowns, Bridges, and more. An example is IPS e-max Press.[6]
Polycrystalline ceramics
Zirconia ceramics: Zirconia ceramics are widely used in modern dentistry due to their high strength, reduced brittleness, and acceptable esthetics. The conventional zirconium oxide material exhibits phase transformation at room temperature, making it unstable. To address this issue, various divalent oxides have been added, with Yittrium Stabilized Zirconia ceramic proving to be the most effective. Depending on the concentration of Yittrium, different types of zirconia ceramics are available:
3 mol%: Offers high strength but compromises esthetics, for example, IPS e-max ZirCad LT
4 mol%: Provides better esthetic outcomes, such as IPS e-max ZirCad MT
5 mol%: Offers the best esthetics but with the least strength, like Cercon XT
The phase transformation toughening characteristic of zirconia ceramics helps to halt crack propagation, giving them a clinical advantage over other materials. These ceramics are commonly used in Fixed Dental Prosthesis, Post & Core, Crowns, Bridges, and other dental applications. There are three main types of zirconia ceramics available for clinical use:
Layered Zirconia: This traditional form involves coating the zirconia structure with a thin layer of porcelain to enhance esthetics, though it may compromise the strength of the restoration.
Monolithic Zirconia: A full-contour zirconia crown with high strength and good esthetics, suitable even for high-stress areas.
Anterior Zirconia: The most recent development, specifically designed for anterior restorations with a focus on esthetics.[7]
Glass + polycrystalline ceramics
Zirconia-reinforced lithium silicate ceramics: ZLS ceramics are ceramic computer-aided design/computer-aided manufacturing (CAD-CAM) materials that have been specially designed. These materials consist of a mixture of Lithium Metasilicate and 10% Zirconium oxide crystals. One of the key advantages of ZLS ceramics is their excellent mechanical properties combined with favorable optics. In fact, studies have demonstrated that ZLS ceramics exhibit superior mechanical properties compared to conventional Lithium Disilicate materials. Furthermore, the biocompatibility of ZLS ceramics has been confirmed by the North American Science Associates Inc. Another noteworthy feature of these ceramics is their versatility in terms of luting options, as they can be luted using both Glass Ionomer Cement and Self-adhesive resin luting material. Commercially, ZLS ceramics are available as CAD/CAM blocks under the brand names Vita Suprinity and Celtra Duo. It is worth mentioning that Vita Suprinity has smaller metasilicate crystals, resulting in higher strength.
Celtra press system: The Celtra Press System comprises pressable ceramic materials that are primarily composed of Lithium Disilicate, along with nanoscale Lithium Phosphate and 10% Zirconium oxide. These materials exhibit a high strength of approximately 500 MPa, making them less prone to marginal chipping. The Celtra Press System can be effectively utilized for fabricating various dental restorations, including Inlays, Onlays, Veneers, and Crowns.
Resin matrix ceramics
Nanoceramics: Comprising 80% ceramic material and 20% resin material with ultrafine particles measuring less than 100 nanometers in diameter, nanoceramics exhibit enhanced mechanical properties. These properties include reduced brittleness, high resilience, minimized natural tooth wear, elevated flexural strength, and improved esthetic outcomes. Nanoceramics are suitable for Inlay, Onlay, and Veneer restorations and can even be utilized in the fabrication of long-span porcelain bridges due to their reduced brittleness.
However, recent research has cautioned against using nanoceramics for crown applications. The high resilience of nanoceramics can result in stress concentration on the thin margins of the crown, leading to potential chipping issues.
Polymer infused ceramic network (PICN): Hybrid ceramic materials, also known as PICN, consist of polymer crystals embedded in a sintered leucite ceramic matrix. While PICN materials exhibit superior mechanical properties compared to traditional feldspathic ceramics, they are considered inferior to other ceramic materials. Noteworthy advantages of PICN materials include potential biomimicry due to their hardness similar to natural enamel, as well as excellent marginal sealing attributed to the presence of resin material.
However, the dual-phase nature of PICN materials limits their use under high loads exceeding 500 N, as this can lead to phase separation and subsequent restoration failure. A commercially available PICN CAD/CAM block, Vita Enamic, has been successfully utilized for creating veneer restorations as thin as 0.2 mm, offering a viable alternative to conventional ceramics to prevent chipping.
Zirconia-silica ceramic within a resin interpenetrating matrix: The combination of zirconia ceramics and silica crystals, which are incorporated into a Bis-GMA or TEGDMA matrix, has demonstrated satisfactory marginal adaptability in clinical settings. These materials are commercially accessible under the name PARADIGM MZ100.
Advancements in ceramic processing techniques
To keep pace with the rapidly evolving technology landscape, the processing of ceramic materials has undergone significant transformations from the traditional powder-liquid slurry method. Modern techniques such as CAD-CAM processing and 3D printing of ceramics have revolutionized the field of dentistry, enabling the creation of faster and more precise restorations.
Innovative processing methods such as hot ceramic pressing and slip casting have been specifically tailored for different ceramic microstructures. Let us now delve into some of these cutting-edge processing techniques.
Slip casting of ceramics
Introduced in the 1990s, slip casting involves the formation of a porous core through slip casting, which is then sintered and infiltrated with a lanthanum-based glass. This results in the development of two interpenetrating continuous networks, a glassy phase, and a crystalline phase. Ceramics manufactured using this method are renowned for their reduced processing defects and enhanced strength compared to traditional feldspathic ceramics.[8]
Heat pressed ceramics
In this approach, powdered glasses are initially sintered and crystallized, shaped into tooth structures at a moderate temperature, and then subjected to final crystallization. This processing technique has been specifically applied to leucite-based and lithium-disilicate-based glass ceramics. The ceramic ingots produced through this method yield final restorations with precise tooth shapes and unique characteristics such as exceptional high bending strength, high fracture toughness, machinability, and a natural esthetic appearance.
CAD-CAM processing
The process of manufacturing ceramic restorations through CAD-CAM consists of three main steps: Data acquisition, restoration design, and restoration fabrication, in that specific sequence. The advent of chair-side ceramic manufacturing has enabled the delivery of restorations within a single day.[9]
The acronym CEREC stands for Chair Side Economical Restoration of Esthetic Ceramics and is the most commonly utilized direct CAD-CAM system. The initial CEREC 1 system has undergone significant advancements to evolve into the current CEREC 5.4 system, which incorporates automatic detection software for restoration type, shade, and insertion axis. In addition, the milling unit has progressed from the traditional 3-axis system to the more advanced 5-axis milling systems, resulting in a more comprehensive final restoration.[10-12]
Cerec Tessera blocks: A novel CAD-CAM ceramic blank, Cerec Tessera Blocks, is a blend of Lithium-Disilicate ceramics and Virgilite material. This material exhibits superior characteristics, including enhanced strength and esthetics due to the cross-linking of Virgilite with disilicate ceramics, and notably, a faster firing time of just 4.5 min owing to the presence of pre-sintered Virgilite crystals.[13-15]
3D printing and additive manufacturing
A recent advancement in the field of dental ceramics is the ability to additively manufacture materials through 3D printing. This method minimizes material wastage while providing restorations with exceptional marginal adaptation and production accuracy surpassing that of milled ceramics. Various techniques for additive manufacturing of ceramics have been identified, with the lithography-based ceramic manufacturing (LCM) technique patented by Lithoz being the most widely accepted. The LCM technique utilizes photopolymerization principles to construct the prosthesis on the Z-axis through vat polymerization, with a vat platform where a ceramic slurry is deposited being a key component of this approach.[16-18]
Advancements in the use of dental ceramics
Advancements in the use of dental ceramics have revolutionized modern dentistry, particularly in the field of restorative materials. Among these ceramics, one of the most versatile materials is porcelain, which has found widespread application in the fabrication of crowns. Initially, porcelain fused to metal crowns were developed to address the esthetic concerns associated with conventional metal crowns. However, with recent technological and microstructural advancements, all-ceramic crowns have emerged as the preferred choice for restorations in the esthetic region.[19-21]
Zirconia implants
In addition to crowns, dental ceramics have also made significant progress in other procedures. One notable advancement is the use of zirconia implants. These implants offer a metal-free alternative with exceptional strength and biocompatibility. Moreover, they are esthetically superior and exhibit a friendly interaction with soft tissues. Studies have shown that zirconia implants have lower bacterial accumulation compared to conventional titanium implants, resulting in reduced peri-implant mucositis after placement.[22-24]
Despite their advantages, the clinical use of zirconia implants has been limited due to certain drawbacks. These include a higher incidence of fractures, which is attributed to the rigidity of zirconia. In addition, zirconia implants are a one-piece cement-retained system, allowing for minimal post-insertion adjustment without failure. Furthermore, the cost of zirconia implants is relatively higher compared to other options.
To address these limitations, a new zirconia implant system called NobelPearl has been introduced. This system consists of a two-piece implant with screws made of carbon fiber and a body made of Alumina toughened Zirconia material (ATZ). The incorporation of carbon fiber with ATZ reduces the rigidity of the implant, minimizing the risk of fracture. Furthermore, the patented Zerafill Osseointegration surface of the NobelPearl implant enhances its stability and longevity within the bone.
In conclusion, advancements in the use of dental ceramics have expanded their applications beyond traditional crowns. The introduction of zirconia implants, such as the NobelPearl system, has provided a metal-free and esthetically pleasing option with improved biocompatibility. While challenges remain, ongoing research and development in dental ceramics continue to enhance their versatility and effectiveness in various dental procedures.
Zirconia abutments
Zirconia abutments are considered a more esthetically pleasing option compared to traditional titanium abutments. However, their clinical application has been restricted due to research indicating that zirconia abutments have lower strength capabilities than titanium abutments. Further studies with extended follow-up periods are necessary to assess the treatment outcomes and ensure proper clinical acceptance of zirconia abutments.[25-28]
Pediatric zirconia crowns
These zirconia crowns are specifically designed for pediatric patients, offering high strength and anatomical precision. Featuring a posterior smart labeling and a universal design for anterior teeth, they are commonly referred to as the “Smart Crown” due to their innovative design. With uniform axial thickness, these crowns require minimal tooth preparation, while multiple retentive boxes ensure excellent retention. The flat inner occlusal surface of the crowns helps distribute occlusal load more efficiently. Manufactured by Kids-e-dental LLP in Mumbai, these crowns are increasingly being utilized in clinical settings.[29-32]
Mandibular cage
The utilization of 3D printing technology in fabricating dental ceramics, combined with the availability of advanced bio-ceramic materials, has revolutionized the application of ceramics in the realm of Oral and Maxillofacial Surgery. In cases where a significant portion of the mandible needs to be removed, a mandibular cage is employed to stabilize the fractured bone ends during the crucial healing phase.
The outer shell of this cage is constructed using high-strength zirconia, which imparts the necessary support during the healing process. Remarkably, this outer shell can remain intact even after the completion of the healing period. On the other hand, the inner pore network of the cage is composed of beta tricalcium phosphate, a material that gradually gets absorbed as the bone regenerates and grows into the pores.[33]
Bioceramics
In recognition of their superior mechanical, biocompatibility, and bioactivity, bioceramics are cutting-edge ceramic materials used in dentistry to replace, restore, or augment biological activities. They are appropriate for a range of dental applications since they blend in nicely with the surrounding tissues.[34]
Utilised as sealants, perforation repair materials, and apical plug materials for root-end fills during root canal therapy.
Dental Prosthetics and Implants Bioactive ceramics, like bio-glass and hydroxyapatite, encourage osseointegration, which increases the stability and durability of implants.
Maxillofacial Reconstruction and Bone Grafting Bio-ceramic materials support facial reconstruction procedures, periodontal regeneration, and bone defect healing.
Dentistry that is Restorative and Regenerative Because they promote tissue repair and regeneration, they are utilised for pulp capping, pulpotomy, and dentin replacement.
Hybrid ceramics
Hybrid ceramics have revolutionized dentistry by offering a combination of strength, durability, and aesthetic appeal. These materials blend ceramic and polymer components to create dental restorations that mimic the natural appearance of teeth while providing superior mechanical properties. Hybrid ceramics are commonly used for crowns, bridges, veneers, and inlays/onlays due to their excellent wear resistance and biocompatibility.[35]
One of the key benefits of hybrid ceramics in dentistry is their ability to be precisely tailored to match the color and translucency of natural teeth, ensuring a seamless and aesthetically pleasing result. Additionally, their flexibility and ease of fabrication allow for more conservative tooth preparation, preserving more of the patient’s natural tooth structure.
Overall, hybrid ceramics represent a significant advancement in dental materials, offering patients long-lasting, natural-looking restorations that enhance both function and appearance.[36]
Nanoceramics
Nanoceramics are ultrafine ceramic particles with sizes less than 100 nm. In dentistry, they offer significant advantages over traditional ceramics due to their enhanced properties such as increased hardness, improved wear resistance, and superior biocompatibility. These materials are used in various dental applications, including fillings, crowns, and implants, providing durable and aesthetically pleasing results.
Their small particle size allows for better integration with natural tooth structures, promoting faster healing and reducing the risk of complications. Additionally, nanoceramics can be engineered to release therapeutic agents, aiding in the prevention of tooth decay and gum disease.
Overall, nanoceramics represent a promising advancement in dental materials, offering improved performance and patient outcomes.[37]
Fiberreinforced composite restorations are a conservative treatment option that can employ ceramics. For patients who are not interested in invasive procedures like full coverage crowns, fiber-reinforced composite fixed partial dentures can be used as a conservative treatment plan. For restorative purposes, thin ceramic crowns made of glass or zirconia ceramics can be used; these ceramics are becoming more sophisticated over time and in response to the needs of clinicians and researchers who are delivering deeper into dentistry.[38]
CONCLUSION
Ceramics, being a highly versatile material utilized in dentistry, boasts a wide range of applications. This has prompted researchers to innovate and enhance the material, leading to the development of more advanced forms. The advent of technology has not only allowed for improvements at the microstructural level but has also opened up new possibilities such as the utilization of 3D printing for ceramics. These advancements have significantly contributed to the progress of dentistry, paving the way for a promising future.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Recent advances in ceramics for dentistry. Crit Rev Oral Biol Med. 1996;7:134-43.
- [CrossRef] [PubMed] [Google Scholar]
- Ceramic materials in dentistry: Historical evolution and current practice. Aust Dent J. 2011;56:84-96.
- [CrossRef] [PubMed] [Google Scholar]
- A new classification system for all-ceramic and ceramic-like restorative materials. Int J Prosthod. 2015;28:227-35.
- [CrossRef] [PubMed] [Google Scholar]
- Advancement of glass-ceramic materials for photonic applications In: Sol-gel based nanoceramic materials: Preparation, properties and applications. Berlin: Springer; 2017. p. :133-55.
- [CrossRef] [Google Scholar]
- Low temperature sintering of fluorapatite glass-ceramics. Dent Mater. 2014;30:112-21.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent Mater. 2016;32:908-14.
- [CrossRef] [PubMed] [Google Scholar]
- Review on transparent polycrystalline ceramics. J Korean Ceram Soc. 2022;59:1-24.
- [CrossRef] [Google Scholar]
- Advances in ceramic matrix composites United Kingdom: Woodhead Publishing; 2018. p. :34-9.
- [CrossRef] [Google Scholar]
- Impact of machining on the flexural fatigue strength of glass and polycrystalline CAD/CAM ceramics. Dent Mater. 2017;33:1286-97.
- [CrossRef] [PubMed] [Google Scholar]
- The evolution of the CEREC system. J Am Dent Assoc. 2006;137:7S-13.
- [CrossRef] [PubMed] [Google Scholar]
- An overview of computer aided design/computer aided manufacturing (CAD/CAM) in restorative dentistry. J Dent Mater Tech. 2018;7:1-10.
- [Google Scholar]
- CAD/CAM Fabricated prosthetic accuracies of lithium disilicate glass ceramic block. Dent Mater. 2022;38:e44-5.
- [CrossRef] [Google Scholar]
- Fracture resistance and failure mode analysis of biomimetic overlays constructed from different machinable blocks and subjected to thermo-dynamic aging. An in vitro study. Egypt Dent J. 2024;70:2695-705.
- [CrossRef] [Google Scholar]
- Translucency of lithium-based silicate glass-ceramics blocks for CAD/CAM procedures: A narrative review. Materials. 2023;16:6441.
- [CrossRef] [PubMed] [Google Scholar]
- A review of 3D printed porous ceramics. J Eur Ceram Soc. 2022;42:3351-73.
- [CrossRef] [Google Scholar]
- Clinical success of the fiber reinforced composite fixed partial denture (FRC FPD) in anterior region for missing one or two missing teeth in anterior region. An original study. J Pharm Neg Results. 2023;14:1856-66.
- [Google Scholar]
- Full mouth reconstruction-malo implant bridge: A case report. Int J Sci Res. 2020;9:1-2.
- [CrossRef] [Google Scholar]
- Structural ceramic components by 3D printing. [International Solid Freeform Fabrication Symposium].
- [Google Scholar]
- Zirconia dental implants: A literature review. J Oral Implantol. 2011;37:367-76.
- [CrossRef] [PubMed] [Google Scholar]
- Current findings regarding zirconia implants. Clin Implant Dent Relat Res. 2014;16:124-37.
- [CrossRef] [PubMed] [Google Scholar]
- A systematic review of the clinical survival of zirconia implants. Clin Oral Investig. 2016;20:1403-17.
- [CrossRef] [PubMed] [Google Scholar]
- Zirconia abutments in the anterior region: A systematic review of mechanical and esthetic outcomes. J Prosthet Dent. 2019;121:775-81.
- [CrossRef] [PubMed] [Google Scholar]
- Zirconia abutments and restorations: From laboratory to clinical investigations. Dent Mater. 2015;31:e63-76.
- [CrossRef] [PubMed] [Google Scholar]
- Zirconia as a dental implant abutment material: A systematic review. Int J Prosthod. 2010;23:299-309.
- [Google Scholar]
- The implant-abutment interface of alumina and zirconia abutments. Clin Implant Dent Relat Res. 2008;10:113-21.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical evaluation and parental satisfaction with pediatric zirconia anterior crowns. Pediatr Dent. 2016;38:192-7.
- [Google Scholar]
- Surface, microstructural, and mechanical characterization of prefabricated pediatric zirconia crowns. Materials. 2019;12:3280.
- [CrossRef] [PubMed] [Google Scholar]
- Zirconia crowns for primary teeth: A systematic review and meta-analyses. Int J Environ Res Public Health. 2022;19:2838.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing titanium grid scaffold facilitates osteogenesis in mandibular segmental defects. NPJ Regener Med. 2023;8:38.
- [CrossRef] [PubMed] [Google Scholar]
- 3D printing assisted finite element analysis for optimising the manufacturing parameters of a lumbar fusion cage. Mater Des. 2019;163:107540.
- [CrossRef] [Google Scholar]
- 3D printed bioceramic scaffolds: Adjusting pore dimension is beneficial for mandibular bone defects repair. J Tissue Eng Regener Med. 2022;16:409-21.
- [CrossRef] [PubMed] [Google Scholar]
- Design and 3D printing of integrated bionic porous ceramic maxillofacial prosthesis. J Mater Sci. 2022;57:20366-79.
- [CrossRef] [Google Scholar]
- Ceramic materials for 3D printing of biomimetic bone scaffolds-Current state-of-the-art and future perspectives. Mater Des. 2023;231:112064.
- [CrossRef] [Google Scholar]
- Options for replacing a single lost anterior tooth in a dentition with reduced periodontal health. J Acad Dent Educ 2024:1-5.
- [CrossRef] [Google Scholar]







