Translate this page into:
Coronavirus disease 2019 safety strategies to be included during dental practice
*Corresponding author S. Krishna, Department of Oral Pathology and Oral Microbiology, Vinayaka Mission’s Sankarachariyar Dental College, Vinayaka Mission’s Research Foundation (Deemed to be University), Salem, Tamil Nadu, India. krishnasmith99@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Varghese AM, Krishna S, Ramesh M. Coronavirus disease 2019 safety strategies to be included during dental practice. J Academy Dent Educ 2020;6(1 & 2):27-34.
Abstract
Coronavirus disease 2019 is caused by SARS-CoV-2 that leads to severe acute respiratory disease. It was first identified in Wuhan City, China, in December 2019 and has resulted in an ongoing pandemic. As of September 15, 2020, more than 26.5 million cases have been reported across the world, with more than 873,000 deaths. As SARS-CoV-2 is highly infective through air-borne contamination, the risk of infection in the dental setting is a serious problem for dental professionals as well as patients. The article provides information on this virus transmission and emphasizes the safety protocols to be followed before, during and after dental treatment.
Keywords
SARS-CoV-2
Coronavirus disease 2019
Dental procedures
Infection control
Teledentistry
INTRODUCTION
Wuhan City, China, first started showing cases of pulmonary disease, with unknown etiology, by the end of 2019. The World Health Organization declared it as a pandemic on March 11, 2020 as the disease started spreading worldwide. The pandemic, coronavirus disease 2019 (COVID-19) caused by SARS-CoV-2, has created a massive crisis among global healthcare and economic welfare.[1] As SARS-CoV-2 is highly infective through air-borne contamination, the risk of infection in the dental setting is a serious problem for both practitioners as well as patients.[2] As the concern of COVID-19 rises, it is very important to practice safety protocols and sterilization methods to keep everyone from the impact of the disease. This article provides a description on the mode of transmission of SARS-CoV-2 virus and the safety measures to be followed.
TRANSMISSION
The possible mode of transmission of SARS-CoV-2 virus is between people who are in close contact with another (around 6 feet) through respiratory droplets released when the infected one coughs, sneezes, or talks.[3] The other routes of transmissions, including the possibility of air-borne transmission, are only being studied since COVID-19 is a new disease. SARS-CoV-2 causes respiratory illness ranging from mild disease to severe disease and death, and there are cases where virus-infected people never develop symptoms.[4] Due to exposure with micro-organisms derived from the oral cavity and saliva, dental health care professionals and patients are at high risk of cross infections.[2] Moreover, the use of rotary and surgical instruments produces a visible spray with droplets of water, saliva, blood, micro-organisms, and other debris that can overcome the protection produced by surgical masks.[3] The highest levels of contaminants can be found within 60 cm from the patient’s head, mainly on the right-hand side of dentists, their masks, around the nose and eyes, says the study done on a mannequin fitted with phantom jaw and seated on a dental chair [Figure 1].[2,5] Furthermore, an in vitro study showed that the viability of SARS-CoV-2 virus in the air is for minimum 3 h and half-life for about 1 h. All surfaces and instruments should be considered as a potential source of virus transmission due to the great adherence of viruses to these for a maximum of 9 days.[2]
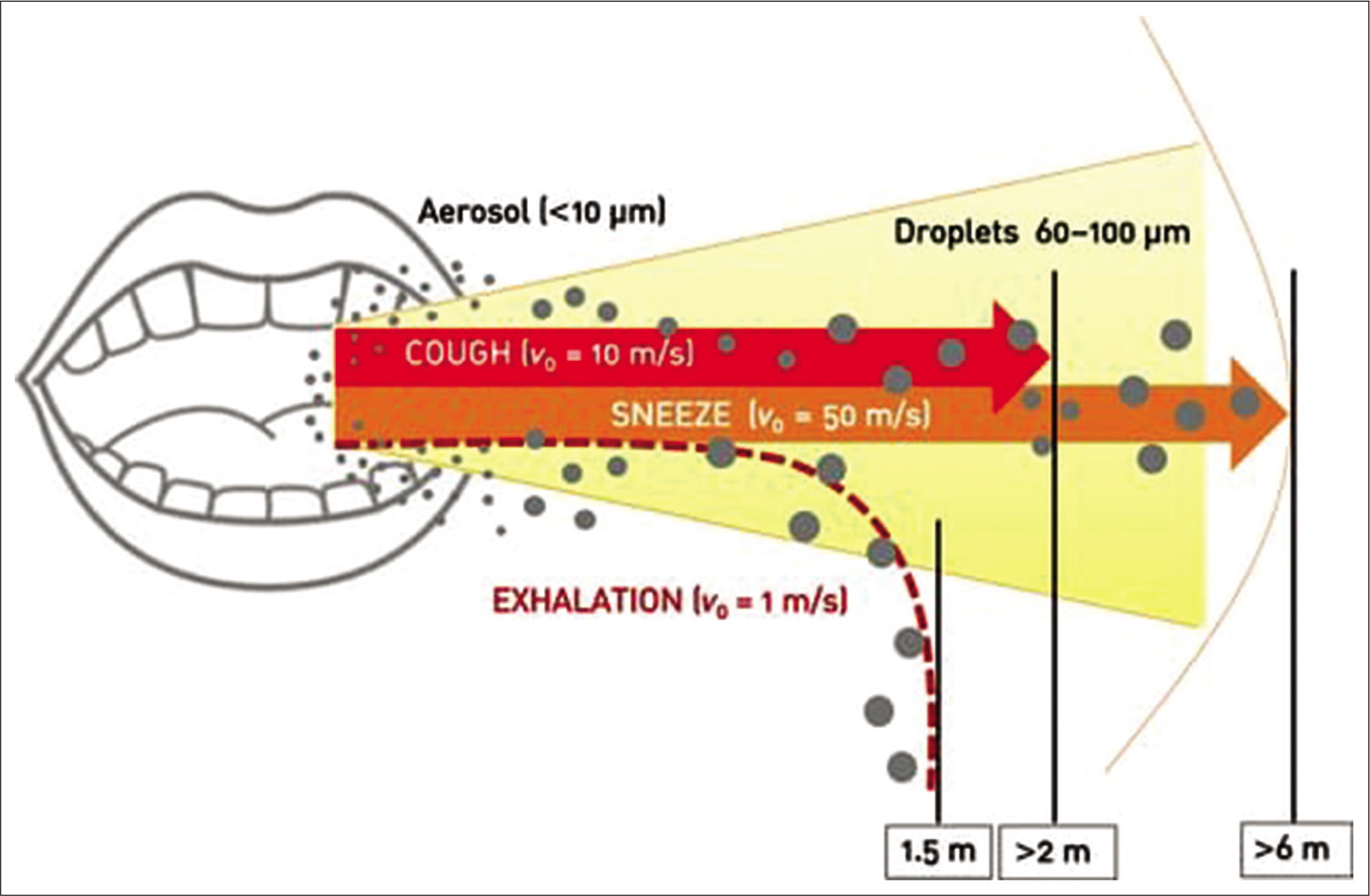
- Exhalation distances of aerosol microparticles and large droplets (original picture with data taken from Xie et al.).
There are people who are not aware that they are affected by the virus, people who purposefully conceal the presence of infection and some not aware of the complexity of the pandemic. This emphasizes the importance to have a series of safety protocols to be followed this time of pandemic.
INFECTION PREVENTION AND CONTROL PRACTICES
Pre-procedure
Teledentistry
Teledentistry can be of great help in the current pandemic situation. It is a combination of telecommunications and dentistry that includes dental consultation and treatment planning over information-based technologies and communication systems.[6] Telephone screening and triage of all patients should be done before the appointment. After considering the signs and symptoms of the patient, a decision should be made by the dentist regarding the emergency of the situation and whether it is necessary for the patient to visit the clinic or not.[7] Appropriate pharmaceuticals, along with home care instructions, should be provided by means of teledentistry if it is not an emergency.[7]
Given below is a table based on the information provided by the American Dental Association (ADA) that helps to decide what constitutes a dental emergency [Table 1].[8]
| Dental emergencies | Urgent dental care | Non-emergency dental procedures |
|---|---|---|
| • Uncontrolled bleeding | • Severe dental pain | • Initial or periodic oral examination |
| • Cellulitis | • Pain in the third molar | • Routine dental cleaning |
| • Trauma involving facial | • Osteitis succeeding surgical procedure | • Aesthetic dental procedures |
| • Localized abscess | • Extraction of symptomatic teeth | |
| • Tooth fracture which causes pain or soft tissue trauma | • Treatment of asymptomatic carious lesions | |
| • Dental trauma with avulsion or luxation | • Orthodontic procedures other than those to address acute issues like pain, infection, trauma |
Waiting room
Dental health care providers should try to limit the number of patients at a time to one and all patients should wear facemasks. Social distancing must be maintained and physical barriers must be introduced. Instructions about hand hygiene and respiratory hygiene must be put up as visual alerts at different places of the clinic, like the entrance. Instructions about how and when to perform hand hygiene, how to use and dispose off the tissues and other contaminated items into respective waste bins, after coughing or sneezing, etc., should also be included.[7] Supplies such as alcohol-based hand rub containing at least 60% alcohol, tissues, etc., must be kept for patients to use. Toys, magazines, and other frequently touched objects must be removed from the waiting room since it is tedious and impossible to keep them sanitized at all times.[3]
Preliminary evaluation of patient
COVID-19 patients have a wide range of symptoms, such as fever or chills, cough, shortness of breath or difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea.
These symptoms should be included in a questionnaire which is to be asked to the patient.
The patient’s temperature also should be taken using non-contact forehead thermometer or with cameras having infrared thermal sensors[9]
Patients answering “yes” to any of the survey questions and whose body temperature is >37.5 °C (99.5 °F) should be confined to their home or hospitalized[2]
Patients answering “yes” to any of the survey questions to the survey and whose body temperature is <37.5 °C (99.5 °F) should not be treated for at least 14 days[2]
Patients who have recovered from COVID-19 can be treated 30 days after symptom remission[2]
-
Patients answering “no” to the survey questions and whose body temperature is <37.5 °C(99.5°F) can be treated, but procedures involving aerosol must be avoided.[2]
Given below is a flowchart depicting treatment to be followed after assessment of severity of the condition of patient
DURING THE DENTAL PROCEDURES
Hand hygiene[10]
Hand hygiene should be practiced during key procedures, that is, before and after each treatment session, before and after removal of personal protective equipment (PPE), following the washing of dental instruments, before coming in contact with steam sterilized instruments, and also after cleaning and maintaining decontamination devices used on dental instruments.
This can be achieved by use of mild soaps. Proper drying of hands should be done after washing. The use of disposable towels and tissues is encouraged to prevent recontamination. Skin care with water-based hand cream can be used to avoid cracking of skin. Clean, short, and smooth fingernails should be maintained. Avoid using rings, bracelets, and wristwatches while carrying out dental procedures.
How to use PPE
Impervious gown, facemask, eye protection, and disposable cap constitute PPE.[11] Regardless of emergency/urgency patients do not proceed with any dental treatment without the use of basic PPE and surgical masks.[10]

-
Sequences recommended for dental professional to use PPE before entering the patient treatment area [Figure 2][12]
Perform hand hygiene
Skin should be protected with protected clothing and gown
Surgical mask or respirator should be used
Eye protection goggles or face shield is used
Use of clean sterile gloves
Enter patient treatment area.[3]
-
After completion of dental procedures [Figures 3 and 4][12]
Gloves are to be removed first
Protective clothing or gown is removed
Exit patient treatment area
Hand hygiene practice is done
Remove eye protection
Surgical mask or respirator is removed
Follow hand hygiene.

- Sequence for putting on personal protective equipment (original taken from CDC).

- Sequence of safely removing personal protective equipment example 1 (originally taken from CDC).

- Sequence of safely removing personal protective equipment example 2 (originally taken from CDC).
| COVID-19 questionnaire | Yes | No |
|---|---|---|
| Do you have a history of fever over the past 14 days? | ||
| Do you have a history of respiratory diseases (e.g.: Cough and breathlessness) over the past 1 month? | ||
| Do you have a history of traveling outside district/state/country over the past 1 month? | ||
| Do you have a history of contact with large crowd/gathering over the past 1 month? | ||
| Do you have a history of contact with COVID-19-positive or a positive suspected person over the past 1 month? |
| Well patients | Patients with suspected or confirmed COVID-19 | ||
|---|---|---|---|
| Dental procedures not involving aerosol-generating procedures | Dental procedures that may or are known to produce aerosols | Dental procedures not involving aerosol-generating procedures | Dental procedures that may or are known to generate aerosols |
| • Work clothing, such as scrubs, lab coat, and/or smock, or a gown • Gloves • Eye protection (e.g., goggles, face shield) • Face mask (e.g., surgical mask) |
• Gloves • Gown • Eye protection (e.g., goggles, face shield) • National Institute for Occupational Safety and Health-certified, disposable N95 filtering facepiece respirator |
• Gloves • Gown • Eye protection (e.g., goggles, face shield) • NIOSH-certified, disposable N95 filtering facepiece respirator |
• Gloves • Gown • Eye protection (e.g., goggles, face shield) • NIOSH-certified, disposable N95 filtering facepiece respirator |
As per occupational safety and health administration, during COVID-19 pandemic, following PPE should be used in dentistry.[13]
Rinsing mouth before procedures
The use of virudical mouth rinse such as 1% hydrogen peroxide or 0.2% povidone-iodine before the dental procedure may reduce the pathogenicity of the organism inside mouth.[11]
Safe injection practices
Injections are to be followed in the aseptic area and disinfection of rubber septum with alcohol before piercing is important. One can also use single-use vials.[14]
Radiographs
Practice extraoral radiographs rather than intraoral, as the later may cause stimulate salivation and cough. If a diagnostic intraoral radiograph is a must, most experienced member should take the radiographs.[11]
Role of suction
High volume evacuation suction capable of removing up to 100 cubic feet of air per minute is recommended by ADA, as it removes droplets at the site of oral cavity and reduces aerosolization of particles.[11]
Rubber dam
To reduce aerosol production and particle spread, dental rubber dams can be used with much effect.[11]
Rotary instruments
High-speed dental handpiece with an anti-retraction valve should be used.[11] If commonly employed air-water syringe is used, a Powered Air Purifying Respirator should be best choice or a full face shield with N95 or similar respirator should be followed.[11]
Use of air purifiers
High-efficiency particulate air filters (HEPA, H12 class) are very much effective and protective when compared to air purifiers with fine filters. F6 class filter air purifier is also effective to some extent.[15]
POST-PROCEDURE
Rotation and reuse strategy are being used in many organizations since the coronaviruses tend to lose their viability significantly after 72 h. It involves acquiring a set number of N95 masks (at least 5 as per the CDC), and rotate their use each day, allowing them to dry for long enough that the virus is no longer viable.[7] However, if the masks get contaminated with blood, respiratory, or nasal secretions, they should be discarded.[7]
Floor should be cleaned with 1% sodium hypochlorite and waterlines should be disinfected with 0.01% sodium hypochlorite to reduce the risk of cross infection[7] all biomedical waste that is being generated should be carefully disposed of from time to time through an authorized biomedical disposal agency.[7]
CONCLUSION
Safety measures to be followed during this pandemic are of utmost importance. This article aids in giving information on this aspect. As the research advances and more studies being done, many changes can be done in these safety protocols.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- COVID-19 pandemic a focused review for clinicians. Clin Microbiol Infect. 2020;26:842-7.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 Dentistry-related aspects: A literature overview. Int Dent J 2020:12601.
- [CrossRef] [PubMed] [Google Scholar]
- Corona Virus Disease 2019, Interim Infection Prevention and Control Guidance for Dental Settings during the Coronavirus Disease 2019 (COVID-19) Pandemic. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html [Last accessed on 2020 Aug 28]
- [Google Scholar]
- Transmission of SARS-CoV-2: Implications for Infection Prevention Precautions. Available from: https://www.who.int/news-room/commentaries/detail/transmission-of-sars-cov-2-implications-for-infection-prevention-precautions [Last accessed on 2020 Jul 09]
- [Google Scholar]
- How far droplets can move in indoor environments revisiting the Wells evaporation falling curve. Indoor Air. 2007;17:211-25.
- [CrossRef] [PubMed] [Google Scholar]
- Applications of teledentistry: A literature review and update. J Int Soc Prevent Community Dent. 2011;1:37-44.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19: Changing trends and impact on future of dentistry. Int J Dent 2020:8817424.
- [CrossRef] [PubMed] [Google Scholar]
- What Constitutes a Dental Emergency Chicago, Illinois: American Dental Association; Available from: http://www.ada_covid19_dental_emergency_bds.pdf [Last accessed on 2020 Mar 31]
- [Google Scholar]
- Corona virus disease 19 (COVID-19): Implications for clinical dental care. J Endod. 2020;46:584-95.
- [CrossRef] [PubMed] [Google Scholar]
- IDA Protocol COVID-19. Available from: http://www.covid-19-ida-protocol.pdf [Last accessed on 2020 Aug 30]
- [Google Scholar]
- COVID-19 and the dental profession: Establishing a safe dental practice for the coronavirus era. J Glob Oral Health. 2020;3:41-8.
- [CrossRef] [Google Scholar]
- Centers for Disease Control and Prevention Recommendations for Putting on Personal Protective Equipment for Treating COVID-19 Patients. Available from: https://www.cdc.gov/hai/pdfs/ppe/ppe-sequence.pdf [Last accessed on 2020 Mar 17]
- [Google Scholar]
- COVID-19-Control and Prevention/Dentistry Workers and Employers. Available from: https://www.osha.gov/SLTC/covid-19/dentistry.html [Last accessed on 2020 Aug 30]
- [Google Scholar]
- CDC Oral Health Standard Precautions. Available from: https://www.cdc.gov/oralhealth/infectioncontrol/summary-infection-prevention-practices/standard-precautions.html [Last accessed on 2020 Aug 28]
- [Google Scholar]
- Using an air purifier as a supplementary protective measure in dental clinics during the corona virus disease 2019(COVID-19) pandemic. Infect Control Hosp Epidemiol. 2020;292:1-2.
- [CrossRef] [PubMed] [Google Scholar]






