Translate this page into:
Association between ABO blood group and COVID-19-positive patients in institutional-based hospital, Coimbatore – A cross-sectional study

-
Received: ,
Accepted: ,
How to cite this article: Abhinaya A, Krishnapriya K, Gowri S, Dinakar J, Tryphena A. Association between ABO blood group and COVID-19-positive patients in institutional-based hospital, Coimbatore – A cross-sectional study. J Acad Dent Educ 2022;8:61-5.
Abstract
Objective:
The novel coronavirus disease (COVID-19) has spread globally and caused 6.5 million death as of October 2022. Risk factors for COVID-19 morbidity and mortality include age, sex, smoking, hypertension, cardiovascular disorders, respiratory disease, and diabetes mellitus. Association between ABO blood groups and number of other infections or disease severity following infections such as SARS-COV-1 and hepatitis B virus has been reported. Rh(D) phenotype (positive and negative Rh blood types) is associated with very few diseases compared to ABO blood group. Various articles have reported the association of ABO blood group and COVID-19. Our aim was to investigate if any association exists in between ABO blood group with Rh phenotype and COVID-19 infection in Coimbatore and with the result an awareness among the public should be created to hasten the preventive measure from further encounter of the infection and help the government in taking a proactive approach to fight COVID-19 in the area. Thus, we conducted a study to find out the association between ABO blood group and COVID-19-positive (SARS-COV-2) patients in institutional-based hospital – Coimbatore which was one of the most affected districts in Tamil Nadu.
Materials and Methods:
This is a single-center, retrospective, observational, and cross-sectional study conducted in a private institutional-based hospital in Coimbatore. The data were collected from around 437 patients’ medical records, who were tested COVID-19-positive between October 2020 and November 2021 whose blood grouping was available as part of investigation. Data were analyzed statistically to correlate the association of ABO blood group, Rh phenotype, and COVID-19 infection.
Results:
In 437 COVID-19-infected patients, the ABO blood group displayed a percentage distribution for A, B, AB, and O at 19% (83), 35% (153), 8.5% (37), and 37.5% (164), respectively and 409 (93.6%) were Rh +ve. Among the patients, blood group O 164 (37.5%), followed by blood group B153 (35%) is observed to be significantly associated with COVID-19 susceptibility, whereas blood group A83 (19%) and AB 37(8.5%) showed lower susceptibility for COVID-19 infection.
Conclusion:
This study did not show any statistically significant association of ABO blood group and Rh phenotype seen in relation to COVID-19 infection.
Keywords
SARS-COV-2
COVID-19
ABO blood group
Rh(D) phenotype
INTRODUCTION
COVID-19 is an infectious disease caused by novel coronavirus that was first identified at Wuhan, China, and affected millions of people worldwide.[1] Around 44 million confirmed cases of COVID-19 infection among India population has been recorded.[2] Individuals infected with COVID-19 disease experience mild-to-severe respiratory illnesses.[3] People who are older and immunocompromised tend to have severe illness and require hospitalization for treatment and mortality rate were increased rapidly in the world and were declared a pandemic. Respiratory droplets being the major cause for the disease transmission, with incubation period of 2–14 days with median of 5 days. In India, O blood group is common[4] with Rh positive phenotype. Various studies have shown correlation between ABO blood group and COVID-19 infection.[5] Based on the recent report released, the individuals with blood group O being resistant to COVID-19 infection[5] and blood group A individuals being more susceptible to the infection. This finding gave impetus to do further study on this topic in Coimbatore which is most affected district in the state. Based on our retrospective study in Coimbatore to find out the correlation between the COVID-19 infected patients and ABO Blood Group, the data collected and analyzed will help the government and public to take proactive and preventive measures to prevent the further spread of COVID.
MATERIAL AND METHODS
This is a single-center, observational, retrospective study conducted in a private institutional-based hospital in Coimbatore. Ethical clearance was obtained from the institutional ethical review board. The study included medical records of individuals affected by COVID-19 both vaccinated and non-vaccinated individuals and recovered completely with their blood group in it. Patients with autism and mentally challenged were excluded from the study. The medical records of 437 patients were collected who were tested positive for COVID-19 between October 2020 and November 2021. The data were collected from those patients who were RT-PCR test positive and ABO blood group and Rh phenotype was available as part of their investigation in the medical records. Data obtained from the patient medical records includes blood groups (A,B,AB,O) along with Rh phenotype and gender. Data were analyzed using Chi-square tests, P-value to correlate the association of ABO blood group with Rh phenotype and COVID-19 infection.
Statistical analysis
The data were entered in Microsoft Excel 2016 for Windows. The frequencies and percentages of age in different groups were calculated. Categorical variables for descriptive analysis were expressed as frequency or percentage. Use of Pearson’s Chi-square test was appropriate to ascertain the relationship between the ABO blood group and other independent variables. P < 0.05 was considered statistically significant.
RESULTS
A total of 437 COVID-19-positive patients’ medical records were randomly investigated, to know if there exists association between ABO blood group and COVID-19 infection based on the RT-PCR test positive results. With which a majority of male patients and minority of female patients’ data were obtained. The Rh+ve phenotype is more in males with 63.2% and female with 30.4%.
The ABO blood group displayed a percentage distribution for A, B, AB, and O at 19% (83), 35% (153), 8.5% (37), and 37.5% (164), respectively. Patients with blood group O had the highest (35.2%) level of positive for COVID-19. However, there is no significant relation seen in association of blood groups with COVID-19-positive as data are not equally distributed among blood group.
There are significant results seen between the gender with ABO (P = 0.04) where males (63.2%) have highest Rh+ve than that of females (30.4%).
The ABO blood group displayed a percentage distribution with relation to gender, where males have highest percentages than that of females for A, B, AB, and O at 13.7% (60), 25.4% (111), 5.3% (23), and 24.3% (106), respectively. Male patients with blood group B had the highest (25.4%) than that of females. However, there is no significant relation seen in association of blood groups with gender.
DISCUSSION
The novel coronavirus disease caused severe distress to the health of world population, along with fall in the economy of many countries. Health-care systems did see an overthrow with the advent of this viral infection.[6] The mortality rate had touched 6.5 million people as of October 2022.[1] Asymptomatic cases were also reported when severity of the symptoms in symptomatic patients varied from mild to grievous cases lead to death of many irrespective of age.[7] Although various rules and restrictions were implemented in preventing further spread, the number of cases raised exponentially day by day.[2] With the advent of the vaccine against the deadly coronavirus (COVID-19), there did bring shift in the trend of the disease and its severity.
ABO is the most commonly used and important blood grouping system in healthcare.[8] This blood group has four types, namely, A, B, AB, and O. Many disorders and diseases have been correlated with ABO blood group with their prevalence. Blood group association with rotavirus, noroviruses (NoVs), dengue virus, Norwalk virus, and hepatitis B virus has been reported.[9-12]
COVID-19 infection has also been subjected to have an association with ABO blood group.[13]
According to our study, blood group O (37.5%) followed by B blood group (35%) showed statistically associated with increased risk and AB least susceptible. Although blood group O seems to be riskier, among COVID-positive patient, blood group B also showed more or less similar values [Table 1 and Graph 1]. Furthermore, male predominance was seen in B blood group based on gender [Table 2 and Graph 2].
| Blood group | Rh+ | Rh- | Total | Chi-square | P-value |
|---|---|---|---|---|---|
| A | 77 (17.6%) | 6 (1.4%) | 83 (19%) | 4.035 | 0.672 |
| B | 145 (33.2%) | 8 (1.6%) | 153 (35%) | ||
| AB | 33 (7.6%) | 4 (0.9%) | 37 (8.5%) | ||
| 0 | 154 (35.2%) | 10 (2.3%) | 164 (37.5%) | ||
| Total | 409 (93.6%) | 28 (6.4%) | 437 (100%) |
| Blood group | Males | Females | Total | Chi-square | P-value |
|---|---|---|---|---|---|
| A | 60 (13.7%) | 23 (5.3%) | 83 (19.0%) | 3.544 | 0.315 |
| B | 111 (25.4%) | 42 (9.6%) | 153 (35.0%) | ||
| AB | 23 (5.3%) | 14 (3.2%) | 37 (8.5%) | ||
| 0 | 106 (24.3%) | 58 (13.3%) | 164 (37.5%) | ||
| Total | 300 (68.6%) | 137 (31.4%) | 437 (100.0%) | ||
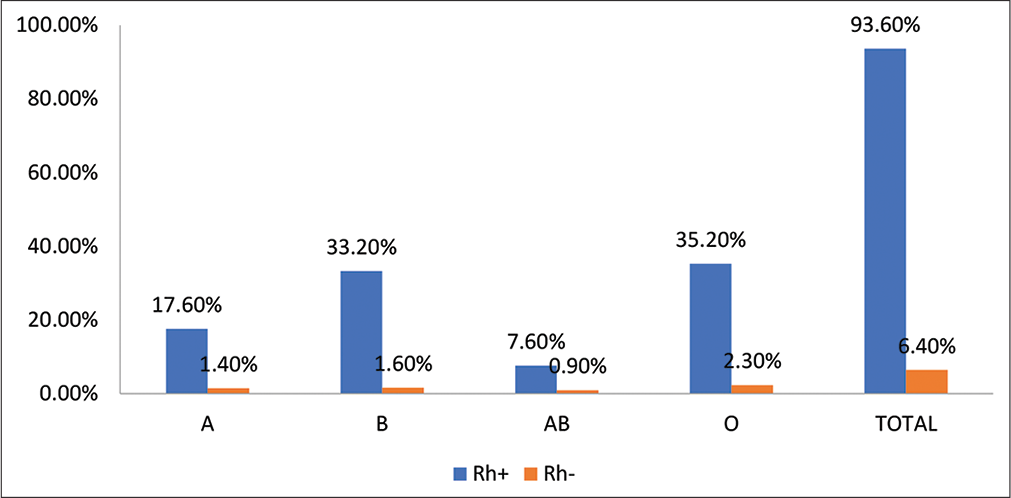
- Association of blood groups with Rh factor.
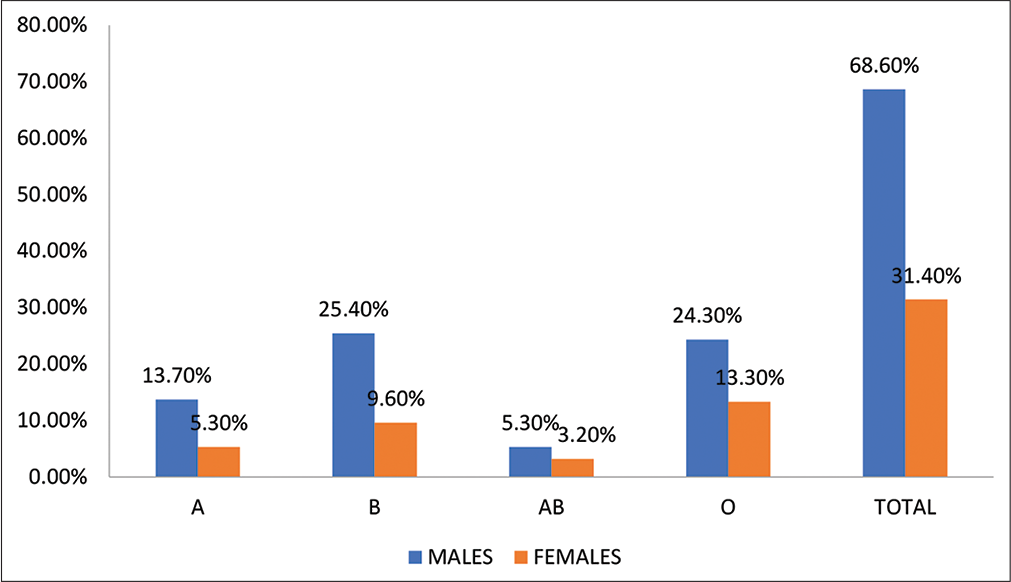
- Association of blood groups with gender.
These data are similar to a study conducted in South-east Asian population, where O blood group patients were prevalent for COVID-19 infection and another supporting study conducted with COVID-19-positive hospitalized patients in USA, reported in their article, there is increased O-positive patients in their population with male gender predominance.[13,14] Our study contrasts with studies conducted by Li et al. on 265 SARS-COV-2 patients, it was observed that blood group A was significantly higher in infected individuals than in the healthy control group population, while blood group O in COVID-19-infected patients was significantly less. Zhao et al. first reported the correlation of ABO blood group with COVID-19 infection[15] whose study showed that there is a risk of infection in A blood group and O blood group individuals are resistant to the infection and several other studies in which A blood group individuals were infected with severity and in whom mortality was high.[16-19] The data [Table 2 and Graph 2] collected supports a study conducted in Iraqi population where, there was high susceptibility of male getting infected for COVID-19 with increased fatality.[20] In our study and study done by Rana et al., blood group B and Rh-positive were more susceptible to COVID-19 whereas AB and Rh-negative were least susceptible to COVID-19 infection.[21]
| Group | Males | Females | Total | Chi-square | P-value |
|---|---|---|---|---|---|
| Rh+ | 276 (63.2%) | 133 (30.4%) | 409 (93.6%) | 4.048 | 0.04* |
| Rh- | 24 (5.5%) | 4 (0.9%) | 28 (6.4%) | ||
| 300 (68.6%) | 137 (31.4%) | 437 (100%) |
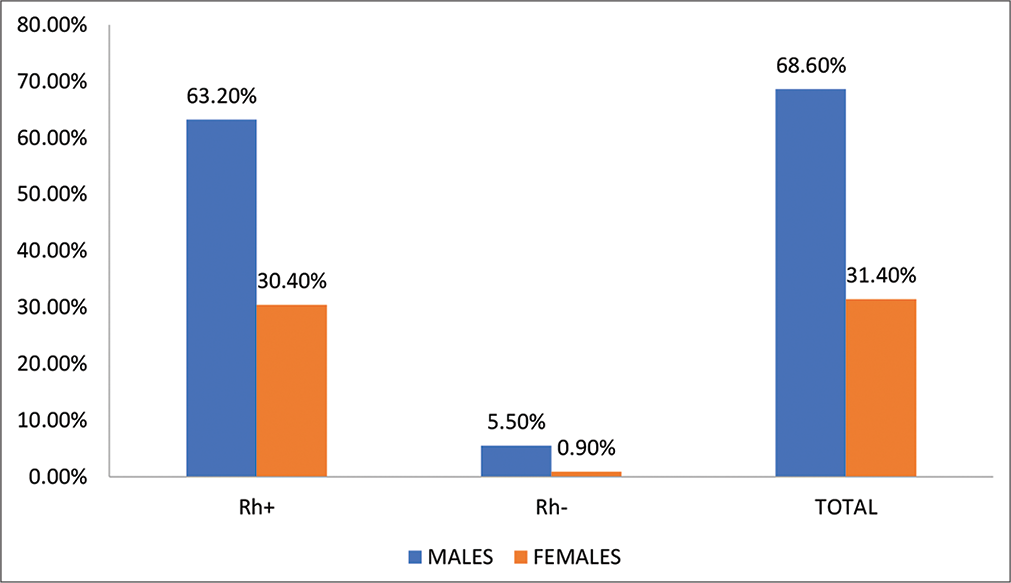
- Association of Rh factor with gender.
Our results [Table 1 and 3; Graph 1 and 3] were in contrast to several studies in which A blood group individuals were commonly infected.[15-18]
Limitation in our study was that it was a single-center and retrospective study conducted in an institutional-based hospital, where various other important data are not collected with limited sample size involved the study.
CONCLUSION
This study did not show any statistically significant association of ABO blood group and Rh phenotype seen in relation to COVID-19 infection. There are several other factors that need to be considered and further investigations are required to confirm their association.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Weekly Epidemiological Update on COVID-19. 2022. Available from: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19 [Last accessed on 2022 Oct 19]
- [Google Scholar]
- Coronavirus (COVID-19) Dashboard. WHO Coronavirus (COVID-19) Dashboard with Vaccination Data. 2021. Geneva: World Health Organization; Available from: https://www.covid19.who.int
- [Google Scholar]
- ABO blood group association and COVID-19. COVID-19 susceptibility and severity: A review. Hematol Transfus Cell Ther. 2022;44:70-5.
- [CrossRef] [PubMed] [Google Scholar]
- ABO and Rh (D) group distribution and gene frequency; the first multicentric study in India. Asian J Transfus Sci. 2014;8:121-5.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between the ABO blood group and COVID-19 susceptibility, severity and mortality in two cohorts of patients. Blood Transfus. 2021;19:54-63.
- [Google Scholar]
- COVID-19 pandemic: From origins to outcomes. A comprehensive review of viral pathogenesis clinical manifestations, diagnostic evaluation, and management. Infez Med. 2021;29:20-36.
- [Google Scholar]
- A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. 2020;54:12-6.
- [CrossRef] [PubMed] [Google Scholar]
- ABO blood groups and hepatitis B virus infection: A systematic review and meta-analysis. BMJ Open. 2020;10:e034114.
- [CrossRef] [PubMed] [Google Scholar]
- ABO blood group and susceptibility to severe acute respiratory syndrome. JAMA. 2005;293:1447-51.
- [CrossRef] [PubMed] [Google Scholar]
- Human ABO blood groups and their associations with different diseases. BioMed Res Int. 2021;2021:6629060.
- [CrossRef] [PubMed] [Google Scholar]
- ABO blood group relationship with COVID-19 occurrence and severity. Indian J Clin Anat Physiol. 2022;9:192-6.
- [CrossRef] [Google Scholar]
- Association of ABO blood group with COVID-19 severity, acute phase reactants and mortality. PLoS One. 2021;16:e0261432.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of ABO and Rh blood type association with acute COVID-19 infection in hospitalized patients: A superficial association among a multitude of established confounders. J Clin Med Res. 2020;12:809-15.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship between the ABO blood group and the coronavirus disease 2019 (COVID-19) susceptibility. Clin Infect Dis. 2021;73:328-31.
- [CrossRef] [PubMed] [Google Scholar]
- ABO blood group predisposes to COVID-19 severity and cardiovascular diseases. Eur J Prev Cardiol. 2020;27:1436-7.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 and ABO blood group: Another viewpoint. Br J Haematol. 2020;190:e93-4.
- [CrossRef] [Google Scholar]
- The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19. Blood Adv. 2020;4:4981-9.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19 and the ABO blood group connection. Transfus Apher Sci. 2020;59:102838.
- [CrossRef] [PubMed] [Google Scholar]
- Association between ABO blood groups and susceptibility to COVID-19: Profile of age and gender in Iraqi patients. Egypt J Med Hum Genet. 2020;21:76.
- [CrossRef] [Google Scholar]
- Association of ABO and Rh blood group in susceptibility, severity, and mortality of coronavirus disease 2019: A hospital-based study from Delhi, India. Front Cell Infect Microbiol. 2021;11:767771.
- [CrossRef] [PubMed] [Google Scholar]






